Understanding Ankylosing Spondylitis
Things to remember | Symptoms | Cause | Diagnosis | Treatment | Medication | Exercise | Self-management | Where to get help | How we can help | More to explore | Download PDF
Things to remember
- Ankylosing spondylitis is a type of arthritis that mainly affects the spine
- There’s no cure, however it can be managed with medication and lifestyle changes
- The most important thing you can do is regular exercise, which helps to keep your spine mobile and flexible.
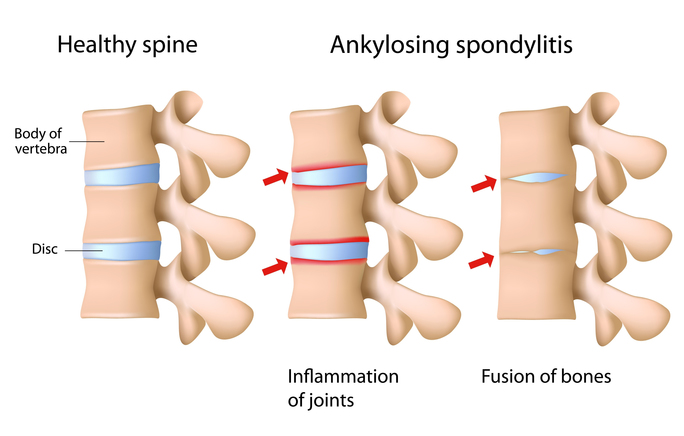
Ankylosing spondylitis (AS) is a type of inflammatory arthritis that mainly affects the spine. Symptoms of AS include back pain, stiffness and reduced mobility in the spine.
The sacroiliac joints are commonly affected in ankylosing spondylitis. These joints connect the base of the spine (sacrum) to your pelvis. Other joints such as the hips and shoulders can also be affected, as can the eyes, skin, bowel and lungs.
Until fairly recently it was thought that AS affected more men than women. However recent research suggests men and women are affected relatively equally.
The symptoms usually appear between the ages of 15 and 45 years. While there’s currently no cure for AS, there are many things you can do to help control your symptoms.
AS is an autoimmune disease. That means that it occurs as a result of a faulty immune system. Instead of identifying foreign bodies (e.g. bacteria, viruses) and attacking them to keep you healthy, your immune system mistakenly attacks healthy tissue in and around your joints causing ongoing inflammation and pain.
In AS, as a result of this inflammation, new bone may grow around the joints in the spine. This can lead to permanent stiffness in the back and neck of some people with AS.
In severe cases this extra bone can fuse the bones of the spine together, however this can usually be prevented by starting appropriate treatment as early as possible.
Symptoms
The symptoms of AS vary from person to person. The most common symptoms are:
- pain and stiffness in the back, buttocks or neck. The symptoms are often worse after rest and relieved by exercise.
- pain in tendons (which connect muscles to bones) and ligaments (which connect bones to each other), often felt as pain at the front of the chest, back of the heel or underneath the foot.
- fatigue (extreme tiredness).
Symptoms may change from day to day. At times your symptoms (e.g. pain, fatigue, inflammation) can become more intense. This is a flare. Flares are unpredictable and can seem to come out of nowhere.
Cause
The cause of AS is unknown. Genes are thought to play a role. You’re more likely to get AS if you have a history of it in your family.
Most people with AS have the gene called HLA-B27, however this gene can also be found in people who don’t have AS. Since the presence of this gene doesn’t automatically lead to the development of AS, other factors are thought to be involved.
Diagnosis
Early diagnosis is important so that treatment can be started as soon as possible. To be diagnosed with ankylosing spondylitis, there needs to be evidence of changes to your sacroiliac joints, in addition to other clinical criteria.
You may undergo a number of tests including:
- medical history
- physical examination
- scans such as x-ray, CT (computed tomography), MRI (magnetic resonance imaging)
- blood tests
- genetic testing.
These tests are generally organised by your doctor or rheumatologist (a doctor who specialises in conditions that affect muscles, bones and joints, or musculoskeletal conditions). They’ll explain what the tests are looking for and what the results mean.
Treatment
There’s no cure for AS, so treatment aims to manage your pain, reduce your risk of complications and improve your quality of life. Your rheumatologist will tailor your treatment to your specific symptoms and the severity of your condition. This can involve trialling different medications to find the medication/s that work best for you.
Medication
Medications used to treat AS include:
- pain relievers (or analgesics) – for temporary pain relief
- non-steroidal anti-inflammatories (NSAIDs) – to control inflammation and provide pain relief
- corticosteroids – to quickly control or reduce inflammation
- disease-modifying anti-rheumatic drugs (DMARDs) – control your overactive immune system
- biologics and biosimilars (bDMARDs) – are biological disease-modifying drugs that work to control your immune system, but in a much more targeted way.
Exercise
Although exercise is important for general wellbeing, it’s especially important in managing AS. Exercise can be used to relieve pain, but is also important for keeping your spine mobile and flexible.
Specific strengthening exercises should be performed to maintain strength through your spine. Exercises performed in warm water (hydrotherapy) can also be helpful.
For overall wellbeing you should also do general strengthening and aerobic exercises. You may find it helpful to see a professional to have an exercise program designed for your specific needs. Consider seeing a physiotherapist or exercise physiologist who specialises in treating AS.
Self-management
There are many things you can do to help yourself:
Learn more about your condition – knowing as much as possible about your AS means that you can make informed decisions about your healthcare and play an active role in managing it.
Exercise and stay active as much as possible – talk with a physiotherapist or an exercise physiologist for specific advice about a daily exercise and stretching program.
Get up and move if you’ve been sitting or standing in one position for long periods at a time (e.g. at work, while travelling).
Learn ways to manage your pain – there are many things you can do to manage pain – and different strategies will work for different situations. For example, heat packs can help ease muscle pain, cold packs can help with inflammation, gentle exercise can help relieve muscle tension. Try different techniques until you find the things that work best for you.
More to explore – watch our excellent videos on pain, your brain and how you can retrain your pain system.
- Pain, the brain and your amazing protectometer – Lorimer Moseley
- Treating pain using the brain – David Butler
Stay involved – in your usual home activities, work, leisure and social activities. Social connections are extremely important.
Be aware of your posture – when sitting, standing and even lying down. Your body should be in correct alignment but also loose and flexible.
Eat a healthy, well balanced diet for general good health.
Manage your stress – it can aggravate your symptoms and make you feel worse.
Acknowledge your emotions – it‘s natural to feel overwhelmed when you’re diagnosed with AS. You may feel scared, anxious, frustrated, sad or angry. It’s important to acknowledge these feelings and get help if they start affecting your daily life. Your doctor can provide you with information about support that’s available.
Seek support from others – you might find it helpful to contact the Ankylosing Spondylitis Group of Victoria and speak to other people who have AS and know what you’re going through. Contact us for information and contact details.
Where to get help
- Your doctor
- Physiotherapist
- Exercise physiologist
- Musculoskeletal Health Australia
Back Pain | Arthritis | Musculoskeletal Conditions (B.A.M) Helpline: 1800 263 265
How we can help
Call our Helpline and speak to our friendly team: phone 1800 263 265 or email helpline@muscha.org
We can help you find out more about:
- ankylosing spondylitis and musculoskeletal conditions
- ways to live well with these conditions
- managing your pain
- read our A-Z guide to managing pain
- watch our excellent videos on pain, your brain and how you can retrain your pain system.
- Pain, the brain and your amazing protectometer – Lorimer Moseley
- Treating pain using the brain – David Butler
- upcoming webinars, seminars and other events
More to explore
- Australian Physiotherapy Association
- Exercise and Sports Science Australia
- Spondylitis Association of America
- NASS—National Ankylosing Spondylitis Society (UK)
- Versus Arthritis (UK)
- Arthritis Foundation (USA)
- Better Health Channel
Download this information sheet (PDF).
The whole or part of this material is copyright to the State of Victoria and the Better Health Channel. Reproduced with permission of the Victorian Minister for Health. Users are permitted to print copies for research, study or educational purposes.
This information has been produced in consultation with and approved by: Musculoskeletal Australia.








