Understanding Rheumatoid Arthritis
Things to remember | Your joints | Symptoms | Cause | Seek advice early for RA | Treatment | Medications | Self-management | Joint surgery | Where to get help | How we can help | More to explore |Download PDF
Things to remember
- Rheumatoid arthritis (RA) causes pain and inflammation in your joints
- It commonly affects the hands, knees and feet
- There’s no cure, but it can be managed and damage to your joints can be reduced with early and ongoing treatment
Rheumatoid arthritis is a chronic condition that results from a malfunctioning immune system.
Your immune system is designed to identify foreign bodies (e.g. bacteria and viruses) and attack them to keep you healthy. However in the case of rheumatoid arthritis, your immune system mistakenly attacks healthy tissue in and around your joints causing ongoing inflammation and pain.
Your joints
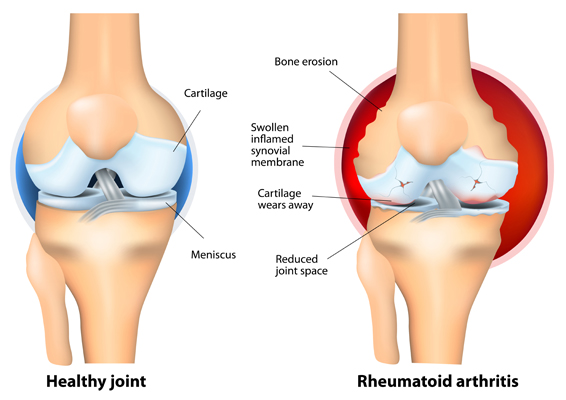
Joints are places where bones meet. Bones, muscles, ligaments and tendons all work together so that you can bend, twist, stretch and move about.
The ends of your bones are covered in a thin layer of cartilage. It acts like a slippery cushion absorbing shock and helping your joint move smoothly.
The joint is wrapped inside a tough capsule filled with synovial fluid. This fluid lubricates and nourishes the cartilage and other structures in the joint.
In RA, the immune system attack on the joints causes a build-up of synovial fluid and inflammation of the tissues that line the joint (synovial membrane). This causes pain, heat and swelling.
Cartilage becomes brittle and breaks down. Because the cartilage no longer has a smooth surface, the joint becomes stiff and painful to move.
Ligaments, tendons and muscles surrounding the joint can also be affected, causing joints to become unstable.
Symptoms
The most common symptoms of RA include:
- swelling, pain and heat in the joints, usually the smaller joints of the hands or feet
- stiffness in the joints, especially in the morning
- persistent mental and physical tiredness (fatigue)
- same joints on both sides of the body are usually affected
- sometimes other parts of the body (e.g. lungs, eyes) may be affected.
Less common symptoms may include weight loss, inflammation of other body parts (e.g. lungs, eyes) or rheumatoid nodules (fleshy lumps below the elbows or on hands or feet).
Rheumatoid arthritis can occur at any age, but usually appears between the ages of 30 to 60. It affects women more often than men.
The course and severity of RA varies from person to person. Symptoms may change from day-to-day.
At times your symptoms (e.g. pain, fatigue, inflammation) can become more intense. This is a flare. Flares are unpredictable and can seem to come out of nowhere.
Cause
We don’t know what causes the immune system to malfunction and attack the joints, however it appears that your genes may play a role. Other factors such as hormones, infection (by an unknown bacteria or virus), emotional distress or environmental triggers (e.g. cigarette smoke, pollutants) may be involved.
Seek advice early for RA
If you’re experiencing joint pain and inflammation, it’s important that you discuss your symptoms with your doctor. Getting a diagnosis as soon as possible means that treatment can start quickly. Early treatment will help you to control the inflammation, manage pain more effectively and minimise the risk of long-term joint damage and disability.
If you’re diagnosed with RA you may be referred to a medical specialist known as a rheumatologist for further investigations and medical treatment.
Treatment
While there’s no cure for RA, there are many strategies to help manage the condition and its symptoms so you can continue to lead a healthy and active life.
Medications
Your doctor or specialist may prescribe a number of different medications depending on your symptoms and the severity of your condition.
Some of the medications you may take include:
- pain relievers (or analgesics) – for temporary pain relief
- non-steroidal anti-inflammatories (NSAIDs) – control inflammation and provide pain relief
- corticosteroids – quickly control or reduce inflammation
- disease-modifying anti-rheumatic drugs (DMARDs) – control your overactive immune system
- biologics and biosimilars (bDMARDs) – are biological disease-modifying drugs that work to control your immune system, but in a much more targeted way.
Depending on your particular symptoms, and how much pain and inflammation you have, you may take one medication or a combination of different medications.
Self-management
There are other things you can do to manage your RA:
- learn about RA – knowing as much as possible about your condition means that you can make informed decisions about your healthcare and play an active role in the management of your condition.
- exercise – will help you maintain muscle strength and joint flexibility, build up stamina and help you manage your pain. Low-impact aerobic activities include exercising in warm water, cycling and walking. Activities like strength training and tai chi are also beneficial. Seek advice from a physiotherapist or an exercise physiologist before you begin an exercise program.
- see a physio – a physiotherapist can provide advice on ways you can modify your activities, show you pain relief techniques and design an individual exercise program for you.
- talk to an OT – an occupational therapist can give advice on pacing yourself and managing fatigue, as well as how to modify daily activities both at home and work to reduce strain and pain on affected joints.
- try relaxation techniques – muscle relaxation, distraction, guided imagery and other techniques can help you manage pain and difficult emotions such as anxiety, and can help you get to sleep.
- Grab a gadget – supports such as walking aids, specialised cooking utensils, ergonomic computer equipment and long-handled shoe horns can reduce pain and fatigue. An occupational therapist can give you advice on aids and equipment to suit you. (link to aids and equipment)
- rest – can help you to manage fatigue and is particularly important when your joints are swollen.
- stay at work – it’s good for your health and wellbeing. Talk to your doctor or allied healthcare professional about ways to help you stay at work or get back to work.
- eat well – while there’s no specific diet for people with RA, it’s important to have a healthy, balanced diet to maintain general health and prevent weight gain and other medical problems, such as diabetes and heart disease.
- complementary therapies – treatments such as massage, meditation or acupuncture may be helpful. Talk with your doctor or rheumatologist before starting any treatment. Fish oil supplements may also be helpful as they contain omega-3 fats. Research suggests omega-3 fats can help reduce inflammation in RA.
Joint surgery
Surgery may be necessary in some cases if the joint is very painful or there’s a risk of losing joint function.
Where to get help
- Your doctor
- Rheumatologist
- Physiotherapist
- Exercise physiologist
- Occupational therapist
- Musculoskeletal Health Australia
Back Pain | Arthritis | Musculoskeletal Conditions (B.A.M) Helpline: 1800 263 265
How we can help
Call our Helpline and speak to our friendly team: phone 1800 263 265 or email helpline@muscha.org
We can help you find out more about:
- rheumatoid arthritis and other musculoskeletal conditions
- ways to live well with these conditions
- managing your pain
- read our A-Z guide to managing pain
- watch our excellent videos on pain, your brain and how you can retrain your pain system.
- Pain, the brain and your amazing protectometer – Lorimer Moseley
- Treating pain using the brain – David Butler
- upcoming webinars, seminars and other events.
More to explore
- Better Health Channel
- Australian Physiotherapy Association
- Exercise and Sports Science Australia
- Occupational Therapy Australia
- Dietitians Association of Australia
- Medicines Line – 1300 MEDICINE (1300 633 424)
Download this information sheet (PDF).
The whole or part of this material is copyright to the State of Victoria and the Better Health Channel. Reproduced with permission of the Victorian Minister for Health. Users are permitted to print copies for research, study or educational purposes.
This information has been produced in consultation with and approved by: Musculoskeletal Health Australia.








