Baker’s cyst – nothing to do with baked goods
August 10, 2022 by Lisa Bywaters

Although it sounds like it, a Baker’s cyst isn’t named after an occupation like housemaid’s knee (prepatellar bursitis), policeman’s heel (plantar calcaneal bursitis) or writer’s cramp (hand dystonia). It has nothing to do with the act of making delicious, delicious bread 🍞 or other baked goods 😋.
Baker’s cysts are named after Dr W.M Baker, the 19th-century surgeon who first described cysts that form on the back of the knee. Their clinical name is popliteal cyst. Often people don’t know they have a Baker’s cyst, especially if it’s not causing pain. However, sometimes they can cause problems.
Your knee – a complex joint
To understand how a Baker’s cyst affects your knee, it’s helpful to know a little about your knee joint. 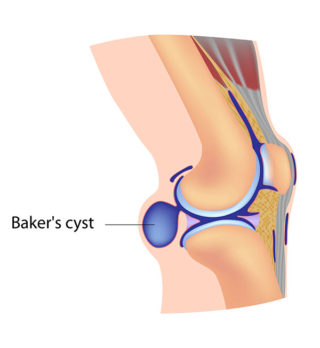
Your knee is a large and complex joint where three bones meet: your thighbone (femur), shinbone (tibia) and kneecap (patella). Covering the ends of your bones is a thin layer of tissue called cartilage. It provides a slippery cushion that absorbs shocks, helps your joints move smoothly and prevents bones from rubbing against each other.
Surrounding the joint is a tough capsule filled with a lubricating fluid (synovial fluid). This fluid allows your knee to move freely.
A Baker’s cyst can form when an injury or arthritis causes your knee to produce too much synovial fluid. This excess fluid bulges from the joint capsule behind the knee as a protruding sac (see image).
Cysts can vary in size and cause symptoms such as pain or stiffness in the knee joint.
Baker’s cysts may not require treatment, but if they do, they can be treated effectively with self-care and medical treatment.
Causes
Some of the common causes of Baker’s cyst include:
- trauma or injury to the knee
- torn cartilage
- osteoarthritis, rheumatoid arthritis and gout.
Symptoms
Often, there are no symptoms, and you may not even know you have a cyst. If symptoms do occur, they can include:
- a lump or swelling behind the knee
- knee pain
- stiffness or tightness of the knee
- limited range of knee movement (if the cyst is large).
Diagnosis
Many people don’t know they have a Baker’s cyst as it may be small and painless.
However, you should see your doctor if you notice a painful lump in the space behind your knee.
Your doctor will ask about your symptoms and medical history and examine your knee. They’re usually able to diagnose a Baker’s cyst based on this.
Sometimes a doctor may organise scans of the joint, usually an ultrasound, or if the diagnosis is uncertain, possibly an MRI (magnetic resonance imaging). This is to rule out other rare causes of the lump, such as a popliteal aneurysm, blood clot or tumour.
Complications
The symptoms of a Baker’s cyst are usually mild; however, in rare cases, the cyst may burst, leaking fluid into the calf region. This can cause increased pain in the knee and swelling or redness in the calf.
If you experience swelling or warmth in your calf, you should seek medical advice quickly.
It can be difficult to tell the difference between the complications of Baker’s cyst and more serious but less common problems such as a blood clot in a vein in your leg. So it’s better to be safe and get it checked out.
Treatment
You probably won’t need treatment if you have no symptoms or only mild pain.
However, if it is causing you pain, your doctor will develop a treatment plan that may include:
- Self-care. You can reduce the pain and swelling by using an ice pack on your knee for short periods. Make sure to wrap it in a cloth so the pack doesn’t come into direct contact with your skin. You should also protect and rest the joint. Elevate your knee while resting it, and avoid activities that strain your knee (e.g. jogging). You may also find it helpful to use a cane or crutches for a short period or wear a knee support.
- Medicines such as paracetamol or non-steroidal anti-inflammatory medicines (e.g. ibuprofen) may provide temporary pain relief. These medicines are available over-the-counter or with a prescription, depending on their dosage and other ingredients.
A corticosteroid (steroid) injection may be helpful for people who haven’t found relief from other treatments or if they have severe pain. - Treating the underlying condition (e.g. arthritis) is also important, so your doctor may discuss other medicines and treatment options.
- Seeing a physiotherapist or exercise physiologist for gentle strengthening and range of movement exercises to reduce symptoms and maintain knee function.
- Draining the cyst by inserting a needle into it (needle aspiration) and removing the fluid. This may be done under ultrasound.
- Surgery is rarely needed to treat a Baker’s cyst. However, it may be an option in some cases to treat the cause of the cyst (e.g. an injury) or to remove the cyst if all other treatments haven’t provided relief.
Contact our free national Help Line
Call our nurses if you have questions about managing your pain, musculoskeletal condition, treatment options, mental health issues, COVID-19, telehealth, or accessing services. They’re available weekdays between 9am-5pm on 1800 263 265; email (helpline@msk.org.au) or via Messenger.
More to explore
- Baker’s cyst
Mayo Clinic - Baker’s cyst
NHS - Baker’s cyst
Cleveland Clinic - Baker’s cyst (popliteal cyst)
OrthoInfo - Baker’s cyst
Patient - What is a Baker’s cyst (popliteal cyst)?
Medical News Today








