Understanding Bursitis
Things to remember | Symptoms | Causes | Overuse injury | Diagnosis | Treatment | Long-term management | Where to get help | How we can help | More to explore | Download PDF
Things to remember
- Bursitis is caused by the inflammation of a bursa
- Common causes of bursitis include injury and overuse
- Treatment includes rest, ice packs and gentle mobilisation exercises.
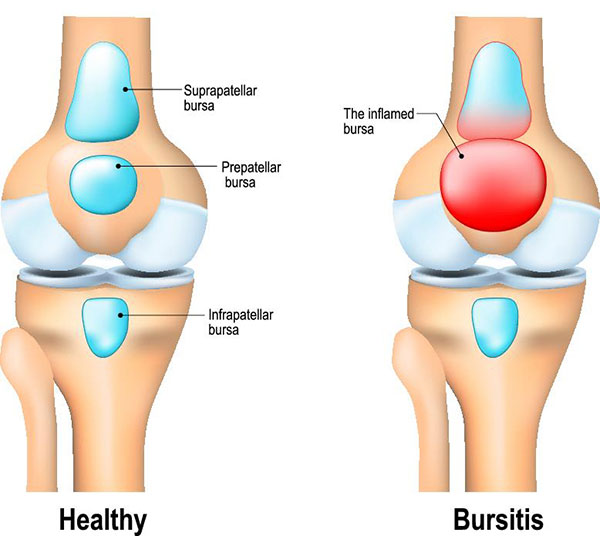
Bursitis is caused by the inflammation of a bursa. A bursa is a small fluid-filled sac that acts as a cushion between your bone and soft tissue (muscles, tendons and skin). A bursa (plural bursae) reduces friction and assists joint movement.
When you overuse or injure a joint, a nearby bursa can become irritated or inflamed. The bursa fills with excess fluid, causing significant pain and restricting movement.
Symptoms
The symptoms of bursitis may include:
- localised pain
- swelling
- a warm feeling in or around the affected area
- increased pain at night
- pain that becomes worse on movement
- stiffness
- reddening of the skin in the affected area.
The shoulder, elbow, hip, knee and heel are the most common sites of bursitis.
Causes
Injury, repeated pressure and overuse are common causes of bursitis. Some conditions, such as rheumatoid arthritis, gout and diabetes, can also contribute to its development. Being overweight can increase your risk of developing hip and knee bursitis.
Bursitis can also be caused by an infection. This may occur if a joint is injured and bacteria get into the bursa.
Overuse injury
A common cause of bursitis is overuse of a joint, especially if the activity is performed awkwardly or with considerable pressure. Doing the same kinds of movements every day or putting stress on joints increases the risk of developing bursitis.
Examples of work-related activities that may trigger bursitis include production-line packing, laying carpet and typing. Sports that can cause bursitis include jogging, tennis and squash.
Diagnosis
Bursitis is generally detected as a tender, warm swelling at the site of a bursa. A diagnosis may include investigating and ruling out any other possible causes.
Tests performed to confirm or rule out bursitis may include:
- physical examination
- medical history
- x-rays, to rule out the possibility of any other condition
- ultrasound
- taking fluid from the bursa to rule out the possibility of infection.
Treatment
Treatment will depend on the cause of the bursitis, and aims to relieve your symptoms as much as possible while the healing process takes place.
Treatment options may include pain-relieving medications, cold packs, gentle mobilising exercises and rest. Anti-inflammatory medications or injections of corticosteroids may be used in cases of severe pain.
If infection is present, as well as pain and swelling of the affected area, you may develop other symptoms, such as a raised temperature. Treatment with an appropriate antibiotic is necessary to treat the infection.
If the bursitis was triggered by a particular form of overuse, it‘s important to avoid that activity, or modify how you perform that activity. An occupational therapist can help you find solutions to this problem.
Correct posture and joint protection are useful, and braces or splints can decrease the stress on the areas and support good alignment.
Long-term management
Your doctor, physiotherapist and/or occupational therapist can offer suggestions and strategies to reduce your risk of developing bursitis again.
To prevent work-related bursitis:
- use ergonomically-designed furniture and equipment
- take regular breaks
- do simple stretching exercises regularly throughout your day
- keep benches at waist height so that your shoulders can relax.
To prevent sport-related bursitis:
- warm up thoroughly by stretching and gently going through the motions of your sport
- make sure you use the correct technique and regularly practise strengthening and conditioning exercises that complement your particular sport
- cool down thoroughly with gentle stretches
- make sure your footwear and equipment are appropriate for you.
Where to get help
- Your doctor
- Physiotherapist
- Occupational therapist
- Musculoskeletal Health Australia
Back Pain | Arthritis | Musculoskeletal Conditions Helpline: 1800 263 265
How we can help
Call our Helpline and speak to our friendly team: phone 1800 263 265 or email helpline@muscha.org
We can help you find out more about:
- bursitis and other musculoskeletal conditions
- ways to live well with these conditions
- managing your pain
- read our A-Z guide to managing pain
- watch our excellent videos on pain, your brain and how you can retrain your pain system.
- Pain, the brain and your amazing protectometer – Lorimer Moseley
- Treating pain using the brain – David Butler
- upcoming webinars, seminars and other events.
More to explore
Download this information sheet (PDF).
The whole or part of this material is copyright to the State of Victoria and the Better Health Channel. Reproduced with permission of the Victorian Minister for Health. Users are permitted to print copies for research, study or educational purposes.
This information has been produced in consultation with and approved by: Musculoskeletal Health Australia.










