Understanding Osteoporosis
Things to remember | Your bones | Normal bone and osteoporotic bone | Diagnosis | Bone health – calcium | Bone health – vitamin D | Bone health – exercise | Falls and fractures | Tips for bone health | Treatment | Medication | Where to get help | How we can help | More to explore | Download PDF
Things to remember
- Osteoporosis means ‘porous bone’
- It causes bones to lose their strength and break more easily than normal bones
- There are things you can do to reduce your risk of developing osteoporosis
- And there are effective treatments for people who have osteoporosis
Osteoporosis is a condition that causes bones to become weak and lose their strength, making them break more easily than normal bones. It affects more women than men.
Your bones
Bones are living tissue that is constantly growing, rebuilding, replacing and repairing.
From birth to about 25 years of age, you build more bone than you lose. Your bones are not only getting bigger as you grow during this time, but they’re developing their density. This determines how strong they are.
From about 25 to 50 years of age your bones break down and rebuild at about the same rate. They’re in a state of balance. This is when you’ve achieved your ‘peak bone mass’. Your bones are at their strongest.
After about 50 years of age, you start to break down more bone than you rebuild. While this means that we will all experience some bone loss, it doesn’t mean that everyone will develop osteoporosis.
Women commonly experience a period of rapid bone loss after the onset of menopause. After this time there is a steady but less rapid loss of bone.
It’s important during all of these stages that you do everything you can to improve our bone health.
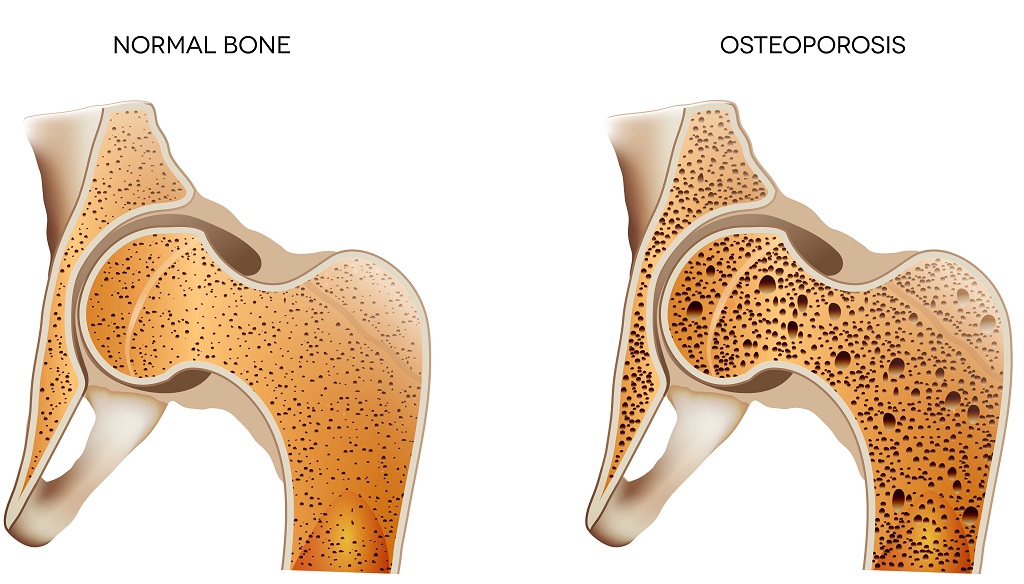
Normal bone and osteoporotic bone
If you were able to look inside your bones, you would see that the inside is a honeycomb-like structure.
In normal bone, the spaces in the honeycomb are small and densely packed. This makes bones strong enough to provide your body with structure and to protect your insides, while at the same time being light enough for you to move around.
When a person develops osteoporosis, the spaces in this honeycomb structure become larger and bone density is lost. This means the bone becomes more fragile. They’ve lost their strength.
Osteoporotic bones break (or fracture) more easily than normal bone. Even a minor bump or fall can cause a serious fracture.
Osteoporosis is often called a silent disease, as there are usually no signs or symptoms until you break a bone.
Diagnosis
If you’re concerned that you may have osteoporosis, or may be at risk of developing it, you should see your doctor.
Your doctor will assess your risk factors for developing osteoporosis, and will look at your medical history – including your family history.
Family history is important because having a parent or sibling with osteoporosis puts you at greater risk of developing osteoporosis.
After assessing your risk factors, your doctor will then decide whether you need to have a bone scan. This scan will measure the density of your bones. The best scan for assessing your bone density is a dual energy x-ray absorptiometry – often referred to as a DEXA or DXA scan.
A DEXA scan uses a low radiation dose (similar to background radiation) to determine how much bone tissue you have. It usually takes about 10-20 minutes and involves a scanning arm that passes over your body to take images of your hips and spine.
Your DEXA test results are reported using T-scores. T-scores show how much your bone density is above or below that of a healthy young adult.
Understanding your T-score:
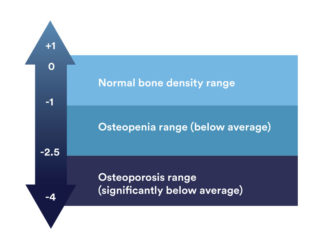
A Z-score may also be used when explaining your DEXA scan results to you. This score compares your bone density to that of someone the same age and sex as you. A Z-score can also be useful for indicating any possible underlying cause of osteoporosis.
Osteoporosis is diagnosed based on the results of your bone mineral density scan. Knowing your bone mineral density, alongside your fracture risk assessment, helps your doctor to work out your overall fracture risk.
Bone health – Calcium
Your bones act as a calcium bank. Most of your body‘s calcium is stored here. If you don’t have enough calcium in your diet, your body will take calcium from your bones. If calcium is constantly taken from your bones, they’ll become weaker over time.
For adults the amount of calcium required each day is between 1000-1300mg – the exact amount depends on your age.
Calcium can be found in lots of foods – including dairy food, oranges, sardines and salmon, almonds, tofu, baked beans, green leafy vegetables.
If you don’t think you’re getting enough calcium through your diet, talk with your doctor. You may need to consider taking a supplement. You can also get advice from a dietitian about ways to add more calcium to your diet.
Bone health – Vitamin D
Vitamin D is produced when your skin is exposed to the sun. It’s essential for strong bones because:
- it helps increase your absorption of calcium
- it helps regulate the amount of calcium in your blood
- it helps strengthen your skeleton
- it can assist with muscle function and reduce your risk of falls.
The main source of vitamin D is sunlight. You should expose your hands, face and arms to the sun every day. The amount of time you need to do this depends on where you live, the time of the year and the complexion of your skin. Healthy Bones Australia has developed a chart to help you work this out.
Vitamin D can also be found in small quantities in foods such as: fatty fish (salmon, herring, mackerel), liver, eggs and fortified foods such as low fat milks and margarine. For most people it’s unlikely that adequate quantities of vitamin D will be obtained through diet alone.
Bone health – Exercise
Apart from having a calcium rich diet, and making sure you get enough vitamin D, regular exercise is important for maintaining healthy bones.
Regular and appropriate exercise strengthens bones and muscles. It also improves balance and flexibility which can reduce your risk of falls and fractures. Doing a variety of different exercises including weight bearing exercises is best as it exercises the bone in different ways.
Exercise also:
- maintains bone health in adulthood
- helps to prevent or slow bone loss after menopause in women
- helps to improve balance and co-ordination to reduce the risks of falls.
If you’re unsure about what exercise is right for you, seek advice from a health professional such as a physiotherapist or exercise physiologist.
Falls and fractures
Osteoporosis has no obvious symptoms, and doesn’t cause pain. However osteoporosis causes bone to become more likely to break. This is what leads to pain, disability and in some cases, loss of independence.
Fractures due to osteoporosis can occur in any bone, however the most commonly fractured are: spine, hip and wrist.
Fractures often occur as a result of a fall. As you age your chance of falling increases. For people with osteoporosis even a minor fall can cause a fracture.
Falls are most commonly caused by:
- poor muscle strength
- poor vision
- problems with balance (due to weak muscles, low blood pressure, inner ear problems, medicines, poor nutrition)
- home hazards which lead to tripping – e.g. rugs, pets, extension cords.
There are things that you can do to reduce your risk of falling. Talk with your doctor for information and advice.
Tips for bone health
There are many things you can do to reduce your risk of developing osteoporosis.
If you have osteoporosis there are also things you can do to improve your bone health, and hopefully prevent your osteoporosis progressing.
Things you can do:
- know your risk – talk to your doctor about osteoporosis. Are you at risk of developing osteoporosis? If you have osteoporosis, is it being managed as well as possible?
- learn about your condition – knowing as much as possible about your condition means that you can make informed decisions about your healthcare and play an active role in managing it
- ensure your diet has enough calcium – a dietitian can help you ensure you’re getting calcium through a variety of different foods
- keep moving and exercise regularly – talk with a physiotherapist or exercise physiologist about an exercise program tailored specifically for you
- falls prevention – if you’ve either fallen before or you feel unsteady and are concerned you may fall, talk with your doctor
- stop smoking – as well as the many other health issues related to smoking, it’s also linked to reduced bone density
- consume in moderation – alcohol, caffeine and salt as they can all affect your bone density. Alcohol also increases the risk of falling, and the chance of fracturing a bone
- have a support team – this may be your family, friends or a peer support group. They can all help you deal with the physical and emotional challenges of living with osteoporosis. There are osteoporosis specific peer support groups, as well as peer support groups for people with a variety of different musculoskeletal conditions, including osteoporosis.
Treatment
Osteoporosis can be effectively managed. The best approach is a team approach which includes you, your health professionals and those closest to you.
Your GP is an important partner in the management of your condition. They can help you manage day-to-day, as well as helping you access other health services.
You may from time-to-time need to see a specialist such as a rheumatologist or an endocrinologist if you’re experiencing complications relating to your condition.
Medication
The type of medication chosen by your doctor depends on factors such as your age, general health and fracture risk.
Osteoporosis medicines work by:
- slowing down bone loss – antiresorptives
- increasing the amount of bone that’s made – anabolic medicines.
Antiresorptives – these are the most commonly prescribed medication for treating osteoporosis.
Anabolic medicine – is used to treat people with severe osteoporosis.
Hormone replacement therapy (HRT) – may be an option for some postmenopausal women. Your doctor will carefully consider the risks and benefits and duration of treatment on an individual basis for HRT.
Supplements – your doctor may prescribe calcium or vitamin D supplements if you’re not getting enough through diet or exposure to sunlight. The Australian Rheumatology Association has developed information sheets on several medications used to treat osteoporosis.
You can also find patient information on the National Prescribing Service website or by calling Medicines Line on 1300 MEDICINE (1300 633 424) 9am to 5pm weekdays.
Where to get help
- Your doctor
- Your rheumatologist or endocrinologist
- Physiotherapist
- Exercise physiologist
- Dietitian
- Pharmacist
- Peer support groups
- Musculoskeletal Health Australia 1800 263 265
How we can help
Call our Helpline and speak to our friendly team: phone 1800 263 265 or email helpline@muscha.org
We can help you find out more about:
- osteoporosis and musculoskeletal conditions
- ways to live well with these conditions
- managing your pain
- read our A-Z guide to managing pain
- watch our excellent videos on pain, your brain and how you can retrain your pain system.
- Pain, the brain and your amazing protectometer – Lorimer Moseley
- Treating pain using the brain – David Butler
- upcoming webinars, seminars and other events.
More to explore
- Better Health Channel betterhealth.vic.gov.au
- Osteoporosis Australia osteoporosis.org.au
- National Prescribing Service nps.org.au
- Australian Physiotherapy Association physiotherapy.asn.au
- Exercise and Sports Science Australia essa.org.au
- Dietitians Association of Australia http://daa.asn.au
- Australian Rheumatology Association https://rheumatology.org.au








