Written by hand therapist Catherine Reid, B.App. Sci, (OT), M.Sci (H&UL rehab), MAHTA (As awarded by the AHTA), CHT(USA)
It’s no secret I love hands! They’re amazing, complex and delicate structures. They help us connect with the world and each other. They allow us to touch, feel, carry objects, pick up kids and perform all kinds of everyday tasks.
That’s why I’m passionate about people being proactive and looking after them.
As an Accredited Hand Therapist* I’m often asked about the things people can do to look after their hands. Here are my top five tips.
1. Look after the skin on your hands
Your skin protects your hands from the outside world. It’s constantly renewing itself. Every time you wash your hands, you rub away dead skin cells. It’s important to look after your skin by keeping it as clean as possible and using a gentle hand wash. In some cases, gloves might be a good idea, for example if you’re using chemicals to clean your shower, or work in a café washing dishes.
Keeping your hands clean isn’t just about them looking good. It’s also about avoiding infections. Anyone who’s had an infection in their hand will tell you it‘s very painful. This is due to the many nerve endings you have in your fingertips. And because you use your hands so often, it’s hard to avoid banging or knocking an infected or injured hand.
An infection can also limit your hand’s movement, which, if left untreated, can become permanent.
Obviously, keeping your hands clean is impossible with some jobs, so keeping the skin in good shape is essential. Using a good moisturiser or barrier cream after washing is recommended to avoid small cracks developing in the skin. These cracks allow dirt and germs to enter your body, increasing your risk of infection.
Keeping your skin hydrated and moist helps keep your skin supple and leads to faster healing.
2. Stay strong
Many people don’t realise they’re losing strength in their hands until they have a functional problem, such as pain when opening a jar or difficulty gripping a doorknob.
That’s why I recommend exercises to strengthen your hands when you start to notice a problem. Many people strengthen their hands by squeezing a ball; if this is the case, I recommend a softer ball so your fingers can move through a greater range when squeezing. A cheap alternative to squeezing a ball is squeezing plumbing insulation. You can buy it by the metre at hardware stores for a few dollars and in different diameters to suit your hand size.
Accredited Hand Therapists can provide you with exercises for specific muscles or to deal with particular issues you’re having. They may use strengthening tools, exercise putty, and/or exercise bands.
3. Keep your joints moving
As the saying goes, ‘motion is lotion’ as far as your joints are concerned, so don’t let them stiffen up!
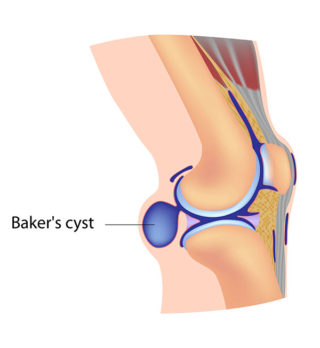
At the ends of the bones in your joints, you have a layer of cartilage. Cartilage is a firm cushion that absorbs shock and enables the bones to glide smoothly over each other. The joint is wrapped inside a tough capsule filled with synovial fluid. This fluid is the oil in your joints. It provides nutrition for the cartilage and helps provide a cushion between the cartilage. It moves across the joint’s surfaces like a drop of oil on a door hinge. When you move your hands, the synovial fluid is spread around the joint. So tasks that have you holding something for a long period without changing grip aren’t good for the joints. It’s not allowing the synovial fluid to lubricate the joint. Rather than not perform the activity, take frequent breaks and move your fingers. And try to avoid activities that push your fingers into extremes of range, for example, lifting items that are too large using only one hand.
Similarly, use bigger, stronger joints where possible. For example, carry shopping bags on your forearm rather than with your fingers.
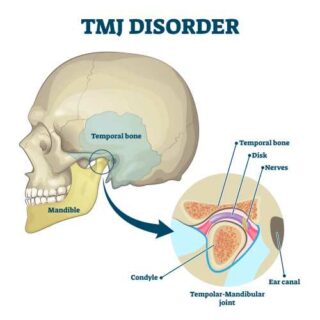
Accredited Hand Therapists can instruct you in exercises for specific joints, such as the joint at the base of the thumb. To maintain good movement, moving your joints through the full range of movement and stretching out to the ends of the range is important. Tendon gliding exercises are often used for this purpose as they glide one set of tendons over the other and move each joint through its full range. Click here for examples of tendon glide exercises.
4. Use the right tool for the job.
We often force our hands into extreme positions or keep going with a task until our hands are aching, especially if we’re in a rush or just want to get a job done.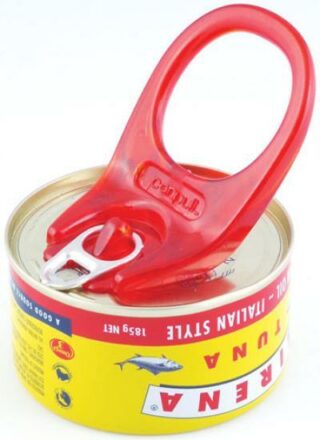
But using the right tools can be gentler on your hands. For example, large or fat handles can spread loads more evenly or over several joints. Tools that use a lever to reduce the required force are also preferable; for example this tool (see image) helps open ring-pull cans.
There are also many electric tools for use in and around the home, reducing the required force. For example, instead of hand pruning a hedge, you can use electric shears. I know which I’d prefer!
You can buy aids and other tools from supermarkets, chemists, hardware stores, and home health care stores. Musculoskeletal Australia also has a range of tools available through their online shop.
5. Seek professional help
If pain or inflammation persists for more than a few days, seek professional help. Pain can be a warning sign that your joints are being overworked. Inflammation can be due to joints, muscles and/or tendons being overused or other health issues such as diabetes or heart disease. Prolonged inflammation can make it difficult to move your fingers. It may be that the structures in your hand need a rest to allow them to heal.
Your GP or a practitioner in hand therapy can help diagnose the problem and provide you with techniques to manage the pain or prevent the problem from becoming worse.
Accredited Hand Therapists can be located via the Australian Hand Therapy Association’s web page under the “Find an Accredited Hand therapist” section.
And check out my other article, ‘Can a hand therapist help you?’.
*As awarded by the Australian Hand Therapy Association
Contact our free national Help Line
Call our nurses if you have questions about managing your pain, musculoskeletal condition, treatment options, mental health issues, COVID-19, telehealth, or accessing services. They’re available weekdays between 9am-5pm on 1800 263 265; email (helpline@msk.org.au) or via Messenger.