Do you get to the end of your busy, tiring day, drag yourself to bed and then have trouble falling asleep? Or staying asleep?
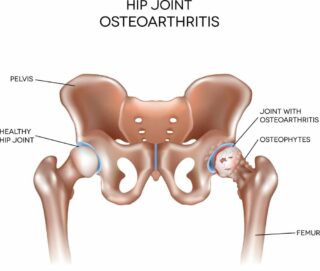
If so, you’re not alone. It’s a common problem, especially for people with musculoskeletal conditions or chronic pain. The Australian Institute of Health and Welfare (AIHW) reports that about two-thirds of Australians aged 18 and over with chronic conditions such as arthritis, diabetes and mental health issues report at least 1 sleep difficulty or problem.(1) And so while it’s probably no surprise to you that poor sleep affects your pain levels and quality of life, did you know it can put you at risk of developing other chronic conditions, including high blood pressure, diabetes and heart disease? (2)
That’s why it’s important to develop a healthy and consistent bedtime routine that allows your body and mind time to wind down and relax so that you can sleep well.
What are the elements of a bedtime routine?
First, a good bedtime routine needs time. Rushing is counterproductive and can lead to more stress and anxiety right before you hop into bed. So give yourself enough time, at least 30 minutes each night. Also, allow time for your new routine to stick. We’re creatures of habit, but when we create new routines, we have to give them time to become second nature.
Next, your bedtime routine should involve things that you enjoy, help calm your body and mind, and let your body know it’s time for sleep.
Here are some suggestions for things you might include in your routine:
- Set a time for going to bed, and stick to it as much as possible. When you have a consistent sleep schedule, your body naturally adjusts and begins to feel tired at the right time each day, making it easier to fall asleep.
- Don’t use technology during your wind-down time. It’s easy to lose track of time while reading emails, checking social media or watching the latest TV series. The next thing you know, you’re still awake at midnight. So put the technology away.
- Write it down and get it out of your head. Put pen to paper and write down your worries, concerns, and things you need to do the next day. Basically, anything playing on your mind and interfering with your ability to relax and sleep. Don’t do this right before you hop into bed, as they’ll still be on your mind. Instead, do it a few hours before bedtime, and then put it away.
- Avoid caffeine, alcohol, nicotine and big meals close to bedtime. They can affect your ability to fall asleep and the quality of your sleep. Instead, drink water, herbal tea or non-caffeinated drinks. And if you’re hungry, eat a light snack, for example, a piece of fruit, some yoghurt or a small handful of nuts.
- Adjust the temperature. Your body’s core temperature needs to drop a few degrees for you to fall asleep. So for your bedroom temperature, it’s best to aim for cooler (but not cold) rather than warm. A helpful tip from the American Academy of Sleep Medicine is to think of your bedroom as a cave: it should be cool, quiet, and dark.
- Have a warm shower or bath an hour or two before bed. This is also about achieving optimum body temperature for good sleep. The shower or bath will initially warm your body, but then as the water evaporates from your skin, you’ll quickly cool down. The warm water also stimulates blood flow from your core to your hands and feet, lowering your body temperature.
- Don’t forget your teeth! While it doesn’t directly relate to sleep quality, it’s part of the winding down process at the end of your day.
- Take your regular medicines (if required).
- Avoid strenuous exercise before bedtime. It raises your temperature and heart rate, making it difficult to fall asleep. Instead, save these kinds of activities for your morning or afternoon.
- Do something you enjoy – for example, read a book, listen to music, talk to your partner/kids/pet. These enjoyable activities create a feeling of calm. They can also improve your mood and help you manage stress and anxiety.
- Try other ways to relax – such as gentle yoga, meditation, stretching, deep breathing and progressive muscle relaxation.
- Have sex! Research suggests that having sex improves sleep, whether you’re alone or with a partner. Orgasm releases several hormones, including oxytocin, which when elevated as a result of sexual intercourse improves sleep quality. Cuddling may also help you fall asleep, as it can make you feel calm and comforted.
- Prep for the next day. Take the stress out of your morning routine by doing some prep the night before. Sort out your lunch, outfit, kid’s homework etc, so you can go to bed feeling confident your morning will start well.
These simple suggestions to help you wind down at the end of your day can help you relax and sleep better. And in the end, we all want to sleep well and feel as refreshed as possible when we wake up. So why not give some of these things a go? You’ve got nothing to lose and so much to gain.
Contact our free national Help Line
Call our nurses if you have questions about managing your pain, musculoskeletal condition, treatment options, mental health issues, COVID-19, telehealth, or accessing services. They’re available weekdays between 9am-5pm on 1800 263 265; email (helpline@msk.org.au) or via Messenger.
More to explore
- 23 ways to revamp your night-time routine
HealthLine - Bedtime routines for adults
Sleep Foundation - Getting a good night’s sleep
Musculoskeletal Australia - How to build the perfect wind-down routine
Sleepstation - How to create a bedtime routine for way better sleep
TechRadar - How to design a better bedtime routine
Sleep.org - How to sleep like a baby as an adult: Steal the bedtime routine of a toddler
Inc - Science says having a regular bedtime is healthy for adults, too
healthline - Sleep problems as a risk factor for chronic conditions
Australian Institute of Health and Welfare
Reference
(1-2) Sleep problems as a risk factor for chronic conditions
Australian Institute of Health and Welfare (AIHW)






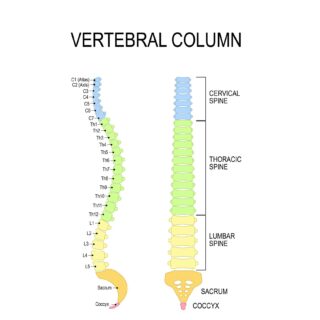 Let’s start with a look at your spine
Let’s start with a look at your spine












