HAND CONDITIONS AND TIPS FOR JOINT PROTECTION
Things to remember | Osteoarthritis | Rheumatoid arthritis | Gout | Psoriatic arthritis | Raynaud’s phenomenon | Carpal tunnel syndrome | Scleroderma | Stenosing tenosynovitis (trigger finger) | Dupuytren’s contracture | Treating hand conditions | Making life easier on your hands | Where to get help | How we can help | More to explore | Download PDF
Things to remember
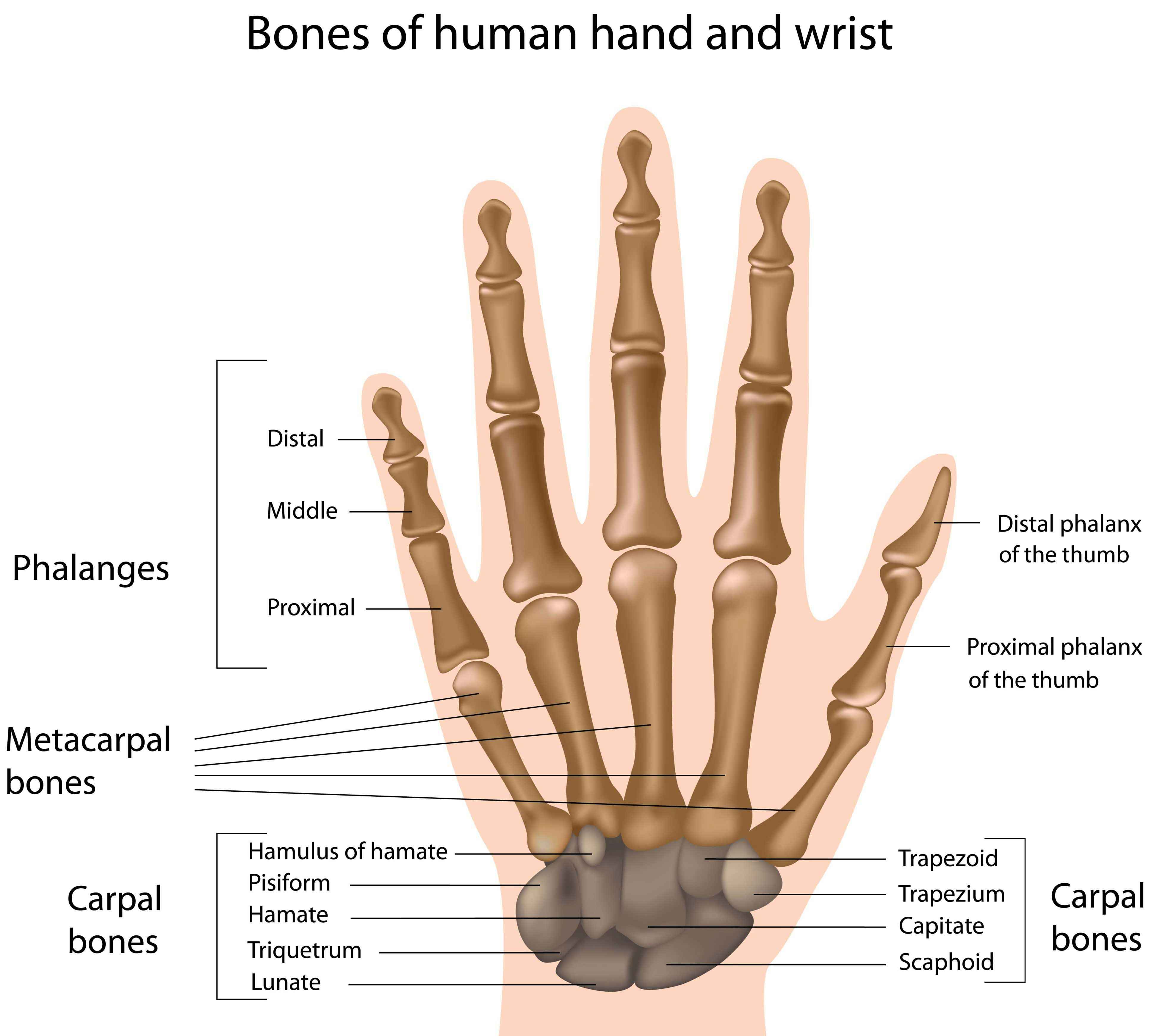
- Our hands are complex and delicate structures
- Each hand has 27 bones, 27 joints, 34 muscles, and over 100 ligaments and tendons
- Conditions such as osteoarthritis and rheumatoid arthritis can cause pain, swelling and sometimes disfigurement in hands
- There are things you can do to decrease hand pain and make everyday activities easier
Arthritis and musculoskeletal conditions that affect the hands can have a great impact on your daily activities and livelihood. This information will look at some conditions that can affect your hands and the things you can do to manage them.
Osteoarthritis
The joints most commonly affected by osteoarthritis are the wrist, finger joints and thumb base. Pain at the base of the thumb can result in difficulty gripping or pinching objects. Fingers may develop ‘bony knots’ called nodes in the middle finger joints (Bouchard’s nodes) or the joints at the end of the finger (Heberden’s nodes).
Rheumatoid arthritis
In rheumatoid arthritis (RA), a chronic inflammatory condition, your immune system mistakenly attacks the thin membrane that lines your joints (synovium). RA often starts in smaller joints such as in the hand or wrist and can cause symptoms such as pain, swelling, inflammation and loss of function. It also usually occurs in a symmetrical pattern e.g. affecting both hands.
Gout
Gout is associated with high levels of uric acid in the blood, causing crystals to form in the joints. A gout attack usually comes on very quickly, often overnight, normally affecting one joint at a time. Affected joints, such as the wrist and joints of the fingers can become red, swollen and intensely painful to touch.
Psoriatic arthritis
Psoriatic arthritis (PsA) is a form of arthritis accompanied by the skin disease psoriasis. Joint involvement can cause inflammation of the entire finger, giving it a sausage-like appearance.
A large proportion of people with PsA experience changes in the fingernails including pitting, thickening and/or separation from the nail bed.
Raynaud’s phenomenon
This condition is caused by a narrowing of the blood vessels to the extremities, usually the hands, in response to cold temperatures or stress. When the blood vessels close down, you’ll notice your fingers change colour. Your fingers may become cold and white, then blue and numb or painful. When blood flow returns, the skin turns from blue to red/purple and finally back to normal pink colour.
Carpal tunnel syndrome
The carpal tunnel is a narrow passageway in the wrist, through which the median nerve runs. The median nerve gives feeling to the thumb, forefinger, middle finger and half of the ring finger. If there is swelling inside the tunnel, the nerve can become compressed.
If this happens you may experience pain, weakness, numbness, and/or pins and needles in the hand and wrist. The pain may also radiate up into your arm and shoulder.
Scleroderma
Scleroderma (or systemic sclerosis) is a chronic connective tissue disease involving the skin and internal organs. Scleroderma literally translated means ‘hard skin’. Although there are several different forms of scleroderma, all can cause thickening and tightening of the skin of the fingers. This can make it harder to bend or straighten the fingers.
Stenosing tenosynovitis (trigger finger)
This condition occurs when the tendon at the base of a finger or thumb becomes inflamed, restricting its ability to move the finger. When this happens, the affected finger/thumb may get stuck in a bent position and may bend or straighten with a snap. Symptoms may include stiffness (particularly in the morning), pain and a popping or catching feeling in the affected finger or thumb.
Dupuytren’s contracture
This is a gradual thickening and tightening of a deep layer of tissue in the palm of the hand (palmar fascia) that extends across the palm to the fingers. Over time this tightening may cause clawing of the fingers as they are pulled towards the palm. Any finger can be involved, however the ring and little fingers are most commonly affected. The typical age of onset for Dupuytren’s contracture is over 50 years, and is seen more often in men than women; particularly those of European descent.
Treating hand conditions
There are many things you can do to look after your hands – whether you have a musculoskeletal condition or not.
Hand care: it’s important to look after your hands. Wash and dry them regularly. Inspect them for irregularities such as swelling, nail and skin changes and any changes to the joint shape or direction of fingers and/or thumbs. By being aware of your hands and any changes that occur, you can seek advice sooner.
Assistive devices: if your hands are painful and stiff you may have difficulty gripping or holding everyday items. Assistive devices such as jar openers, book holders, tap turners, button hook and zipper aids and easy grip utensils can make tasks easier and more efficient by reducing joint stress and eliminating tight grasps. This also includes a range of easy grip garden tools and office equipment. You may need to speak with an occupational therapist about what equipment is best suited to you.
See a hand therapist: if you have hand/wrist pain or a condition that affects your hands, seek the advice and expertise of a hand therapist. Hand therapists are occupational therapists or physiotherapists that have undergone advanced training to become experts in the assessment, diagnosis and treatment of upper limb problems (shoulder to hand). They can provide advice on joint protection and energy conservation (e.g. splints) as well as recommendations for adaptive devices/equipment to improve hand function.
Splints and supports: there are various types of hand splints, gloves or sleeves that can give support to a painful joint by providing mild compression, warmth and/or joint protection. There are two main types of hand or wrist splints – resting splints and working splints. The choice of splint will depend on your condition and your current needs. Splints need to fit your hand comfortably and correctly, so speak with a hand therapist about what’s best for you and how often you should wear them.
Exercise: for healthy joints, you need to keep them moving. Regular hand exercises can reduce stiffness and support your joints by keeping your muscles strong. If you are considering hand exercises, it’s best to get advice from a hand therapist or other specialist as to which exercises are most suitable for you. It is also important to remember that such exercises should be mild and they should not cause you additional pain when you are doing them (see back page for range of motion exercises)
Gloves: if you have Raynaud’s phenomenon, keep your hands warm with gloves. Hand warmers are also helpful.
Medications: depending on the underlying condition causing the problem in your hand/s, your doctor may suggest medications such as analgesics (pain killers) and/or non-steroidal anti-inflammatory medications (NSAIDs). Topical creams and gels are preferred over oral NSAIDs because less medication is absorbed into the bloodstream. Oral NSAIDs can be considered for short-term use. A cortisone injection is not generally recommended for osteoarthritis of the hand, but may be used for rheumatoid arthritis or acute attacks of gout. In conditions such as rheumatoid arthritis you may also be taking disease modifying anti-rheumatic drugs (DMARDs). It’s important to take these medications as prescribed by your doctor.
Surgery: if conservative treatments haven’t helped and your hands remain injured, deformed or there’s a significant decrease in function, surgery may be an option. A referral to a specialist hand surgeon is usually required.
Making life easier on your hands
Sometimes simply changing the way you carry out everyday tasks can help to reduce pain and protect your joints. You can make life easier on your hands by considering the following.
Pain – it can serve as a warning sign that your joints are being overworked. Try to find a balance between activity and rest by pacing yourself. Take regular breaks when completing tasks and try not to overdo it on a good day. You might like to try heat or cold packs to help relieve pain. Some people also like to soak their hands in warm water or wrap their hands around a warm mug of tea. Speak with your health professional to get the right balance of activity for you.
Try to avoid using a tight grip over an extended period of time, for example:
- use foam or sponge to increase the grip size of handles on cutlery, pens and other hand held devices
- use assistive devices with thick rubber grip handles (e.g. key turners, jar openers)
- use rubber squares and gloves to help improve grip
- consider lever handles around your home to minimise any twisting forces e.g. mixer taps in bathrooms/kitchens.
Try to avoid repetitive movements, for example:
- prolonged typing, pruning and power tool usage particularly those that vibrate
- when gardening ensure your tools are sharpened and well maintained for ease of use
- remember to take regular breaks from tasks that require repetitive movements.
Always try to use your body’s larger joints and muscles when you can, for example:
- use your forearms to carry bags instead of your hands
- when carrying items hold them closer to your body
- when lifting heavier items squat and use your thigh muscles.
Spreading the load – try to spread the load of an object over more than one joint, for example:
- when picking up objects use two hands
- slide sheets and swivel pads can help move items with less strain
- divide shopping into smaller bags and try using a backpack and/or trolley.
Finding an alternative – for example:
- buy pre-cut meat and vegetables instead of trying to cut them up yourself
- use electrical items instead of manual e.g. can openers and graters
- look for items that are easier to use e.g. push on pegs
- keep a pair of scissors handy to open packaging
- consider car modifications – read our information on Driving with more comfort and less pain
- ask for help with some tasks.
Rethinking personal care/hygiene – for people with decreased hand function or fine motor skills, everyday tasks such as showering and toileting can be quite challenging. To make things easier you could use:
- a bidet to help with cleaning difficult to reach areas
- baby wipes/moist towelettes instead of toilet paper (but remember that they’re not flushable)
- toilet paper tongs/aids to help with grip
- soap dispensers instead of a bar of soap
- items to make dressing easier e.g. sock sliders, elastic shoe laces, button hole hooks/zip pullers, front fastening bras as well as dressing aids for coats and cardigans
- shoes with velcro fasteners instead of laces.
Before engaging in hand strengthening activities you should discuss this with a qualified hand therapist. This will ensure you are not doing further damage.
Where to get help
- Hand therapist
- Doctor
- Physiotherapist
- Occupational Therapist
- Nurse
- Musculoskeletal Health Australia
Back Pain | Arthritis | Musculoskeletal Conditions (B.A.M) Helpline: 1800 263 265
How we can help
Call our Helpline and speak to our friendly team Monday to Thursday (excluding public holidays). Phone 1800 263 265 or email helpline@muscha.org
We can help you find out more about:
- arthritis and musculoskeletal conditions
- ways to live well with these conditions
- managing your pain
- upcoming webinars, seminars and other events.
More to explore
- Australian Hand Therapy Association www.ahta.com.au
- Australian Physiotherapy Association www.physiotherapy.asn.au
- Better Health Channel www.betterhealth.vic.gov.au
- Arthritis Foundation www.arthritis.org
- American Academy of Orthopaedic Surgeons http://orthoinfo.aaos.org








