Osteoarthritis of the knee
Things to remember | Your knee joint | Symptoms | Causes | Diagnosis | Weight management | Exercise | Medicines | Complementary and alternative therapies | Surgery | Tips for daily activities and living well | Where to get help | How we can help | More to explore | Download PDF | Watch the recording of our webinar on knee osteoarthritis
Things to remember
- The knee is the largest joint in the human body
- Osteoarthritis (OA) of the knee occurs when the structure of the joint becomes damaged
- People over 45 are more at risk, but younger people can be affected too
- Exercise and weight loss are two of the best ways to manage your knee OA
Your knee joint
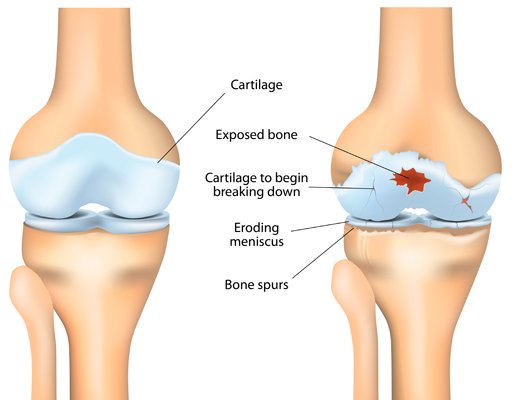
Your knee is a complex weight-bearing joint. It consists of 3 main parts – the end of your thigh bone (femur), the top of your shin bone (tibia) and your kneecap (patella). The end of each of these 3 bones is covered with a slippery surface (called cartilage) which allows your knee to move smoothly.
In between your thigh bone and your shin bone there’s a thickened pad of cartilage called the meniscus. This acts as a ‘shock absorber’ to cushion the two bones and keep the joint stable.
The knee joint is wrapped inside a tough capsule filled with synovial fluid. This fluid lubricates and nourishes the cartilage and other structures in the joint.
Symptoms
The symptoms of knee osteoarthritis usually happen gradually and can include any of the following:
- pain in the knee joint – often worse after vigorous activity and at the end of the day
- pain may radiate up (into the thigh) or down (into the shin) from the affected knee
- stiffness of the knee joint – mainly in the morning or after rest, and which eases in less than 30 minutes or with walking
- swelling of the knee joint – swelling may be soft (caused by additional joint fluid) or hard (caused by bony growths called osteophytes)
- muscle weakness of the thigh or calf
- grinding, creaking or crunching sound when moving the knee
- the knee may feel like it ‘locks’, ‘sticks’ or gives way during periods of activity
- pain is usually eased when resting.
Causes
Your risk of developing osteoarthritis of the knee may be influenced by many factors including:
- age – OA occurs more often in people over 45
- being overweight or obese – extra weight on your knees can increase strain and may lead to premature or increased joint damage
- gender – OA is much more common in women than in men
- previous injury and/or disease of the joint – heavy physical or repetitive activity (e.g. heavy lifting in farming or construction), traumatic injuries (e.g. car accident, sporting injury) or the presence of other diseases (e.g. rheumatoid arthritis, gout) may increase your risk of knee OA
- genetic factors – a family history of knee OA means that you’re at greater risk of developing it yourself.
Diagnosis
Osteoarthritis of the knee can be diagnosed by your doctor without the need for joint imaging such as x-rays or MRI. A diagnosis is normally based on your signs and symptoms such as:
- knee pain during activity
- bony swelling of the knee
- excess fluid around the knee
- restricted movement
- instability of the knee
- joint grating, or creaking/crunching sounds
- weakening of the affected thigh muscle
- stiffness of the joint after rest – less than 30 minutes.
X-rays are not needed for the diagnosis of knee OA but they may be used to assess how much joint damage has occurred. An x-ray can show possible narrowing of the joint space, as well as any bony growths, dislodged bone fragments or calcium deposits. However x-rays are not a good guide as to how much pain you might be in. For some people x-rays show severe joint damage but they have low levels of pain. Others may report high levels of pain with only minor x-ray changes.
Magnetic resonance imaging (MRI) is only required when there is a need to rule out an alternative diagnosis or to assess the health or condition of the soft tissues (cartilage, tendons, muscles) of your knee. MRIs are not recommended in the management of knee OA.
Weight management
Being overweight or obese is known to be directly related to the risk of developing knee OA. It‘s also highly likely to speed up how quickly your OA develops or progresses. Evidence shows that there‘s a relationship between weight loss and relief of symptoms such as pain and stiffness; even a small amount of weight loss (5% of body weight) can improve your symptoms.
Exercise
Exercise is key in the management of knee OA. Professionally tailored exercises by a physiotherapist or exercise physiologist can help reduce your knee pain as well as improve your knee function. Evidence suggests that while there‘s no one particular type of exercise that is better than another, a combination of certain exercises are likely to be the most effective.
These exercises include:
- strength training specifically targeting your legs
- aerobic exercise – these are exercises that get you moving and increases your heart rate (e.g. brisk walking, swimming, cycling) and will help improve the health of your heart and lungs (cardiovascular system)
- balance training
- exercises that move your joint through its full range (range of motion exercises).
When it comes to choosing a type of exercise for yourself think about what you enjoy and what you’re likely to keep doing. The best results occur when you do some sort of exercise at least three times per week. Exercise can be:
- land based (e.g. brisk walking, riding a bike)
- water based (e.g. water aerobics, swimming)
- done in the community (e.g. local exercise class, fitness centre)
- done at home.
If pain is preventing you from exercising, you may find that warm water exercise is a good starting point. Hydrotherapy pools offer the comfort of warmth, as well as the buoyancy of the water to ease the load on your joints. For those that are able, cycling can also provide a good option for non-weight bearing exercise.
Another option is My Knee Exercise, a free 6-month program to help people with knee pain and knee osteoarthritis manage their symptoms. Developed and designed by researchers within the Centre for Health, Exercise & Sports Medicine at The University of Melbourne, research studies have shown that it’s safe and effective. You can try it for free in the comfort of your home today. Simply visit https://mykneeexercise.org.au to access all of the resources and tools to get started.
Medicines
For some people medicines are an important part of managing their OA. Tablets, creams, gels or injections may help to reduce pain and improve function.
There are a variety of medications used in the management of knee OA and each come with varying degrees of evidence to support them. These include:
Non-steroidal anti-inflammatory medicines or NSAIDs (e.g. Nurofen, Celebrex, Voltaren)
NSAIDs are available over-the-counter and with a prescription, depending on their dosage and any other ingredients. They may be taken by mouth (orally) as a tablet or capsule or applied directly to the skin (topical) in the form of gels and rubs.
Oral NSAIDs are considered the preferred first-line drug treatment for OA and have been shown to reduce pain and symptoms in knee OA.
Although there’s no solid evidence either for or against topical NSAIDs it may be worth giving them a short trial to see if they help.
It’s important to note that NSAIDS are designed to be taken at low doses for short periods of time. Always talk to your doctor before starting NSAIDs as they can cause harmful side effects in some people.
Paracetamol
Research has shown that paracetamol (e.g. Panadol, Panamax) provides only low-level pain relief and in some cases no pain relief at all compared to a placebo in knee OA. However some people do report that it helps to reduce or take the edge off their pain so that they can be more active. For this reason, it’s worth discussing a trial of paracetamol with your GP to see if it‘s appropriate for you.
Corticosteroid injections
If you have persistent knee pain and haven’t had relief from oral medication or other treatments (e.g. exercise, weight loss) your doctor may suggest a corticosteroid (steroid) injection. Corticosteroid injections into the knee joint can provide short term pain relief for some people with knee OA. However the duration of pain relief can vary from a few days to a few weeks, and the number of injections you can have is limited due to potential harm. It’s important that you discuss the benefits and risks of steroid injections with your doctor so that you have all the information you need to make an informed decision.
Hyaluronic acid injections
The benefits of hyaluronic acid joint injections (also known as viscosupplementation or hyaluronan injections) are uncertain. Research findings have been inconsistent and although some people do find the treatment helpful, it can be expensive and is not generally recommended.
Opioids
Opioids are powerful pain relieving medications. They’re effective at reducing acute pain (or the pain resulting from an injury or surgery) but evidence shows that they have little effect on OA pain. Opioids also have many potentially serious side effects. That’s why they’re not recommended in the management of knee OA.
Capsaicin
Capsaicin is the active ingredient in chilli peppers – it makes them ‘hot’. Capsaicin in creams and lotions has been used in osteoarthritis to help reduce pain and some people do report beneficial effects. However the evidence for its effectiveness in knee OA is low and it’s not generally recommended. It also has side effects when applied such as a burning sensation which may take several uses to wear off.
Complementary medicines or alternative therapies
Complementary and alternative treatments are widely used by people with musculoskeletal conditions, including osteoarthritis of the knee.
Transcutaneous electrical nerve stimulation (TENS)
A TENS machine is a small battery powered device with leads that connect to sticky pads on your body. It delivers very small electrical currents to your skin that stimulate nerves to relieve pain. Some people find it helpful in relieving pain while others do not. The quality of evidence showing it helps with knee OA is very low. If you’re thinking of using a TENs machine speak with your doctor to see if it’s a suitable option for you. You can often hire one from your physiotherapist, local pharmacy or local hospital.
Electrotherapy
Electrotherapy treatments (e.g. shockwave, laser) are thought to minimise inflammation, promote cell growth and modify pain. While some trials have shown short-term benefits with electrotherapy, the evidence for its use in knee OA is low to very low. For this reason it’s not generally recommended.
Acupuncture
The use of traditional (needle), laser and/or electro acupuncture for knee OA is not supported by current clinical evidence. While some improvements in knee pain and function have been identified in low-quality studies, the benefits are considered so small that they’re not clinically relevant. Also to see any benefits from treatment, it‘s likely that you will need multiple sessions of acupuncture which could become quite costly.
Ultrasound
Therapeutic ultrasound involves a health professional applying high-frequency sound waves to the surface of the skin in order to reach the soft tissues below. There’s moderate quality evidence to suggest that this treatment can reduce pain and improve function in knee OA. However evidence also suggests that you would need three to five treatments a week to see any benefits. For this financial reason, it’s often not recommended.
Glucosamine and chondroitin
Studies have found that there is no benefit from taking glucosamine for osteoarthritis. The Australian Rheumatology Association and the Royal Australian College of General Practitioners recommend against taking glucosamine.
Glucosamine supplements are usually made of shellfish so if you have a shellfish allergy do not take glucosamine. Glucosamine can also affect your blood sugar levels and may adversely affect diabetic, cholesterol, chemotherapy and blood thinning medications.
Much like glucosamine, the effects of chondroitin are unclear. Some studies have found an effect while others did not.
If you’re thinking of trying glucosamine or chondroitin, make sure you speak with your doctor first.
Platelet-rich plasma (PRP) injections
The evidence for PRP is still uncertain. There are large variations in the design of PRP trials and no real standard recommendations for their preparation or use. Until further robust research is undertaken PRP is not recommended for knee OA.
Stem cell injections
Currently there‘s no evidence to support the use of stem cell injections in the treatment of knee OA despite it being commercially available. The International Society for Stem Cell Research and the Australian Rheumatology Association are strongly against their current use for osteoarthritis. It’s recommended that stem cell administration should only take place under a rigorously designed clinical study that prioritises individual health and safety.
Surgery
If you’ve exhausted all non-surgical treatment options and are still experiencing severe pain and reduced knee function, you may want to talk with your doctor about surgery.
A total joint replacement of the knee is the most common type of surgery for knee OA and can provide significant pain relief and improved function. However it’s important to remember that a total knee replacement is major surgery and requires you to commit to months of rehabilitation.
Having an artificial knee means that there will still be some limitations. An artificial knee won’t have the same sideways movement as a natural knee, and it won’t bend fully which means that it’s more likely to be difficult to get down and up from a kneeling position.
Eventually an artificial knee will have to be replaced. The length of time it lasts will depend on many factors including how it’s treated, but it can range from 10 to 20 years.
Arthroscopy is a surgical technique that involves the insertion of small surgical instruments, including a camera, into the knee. This allows the surgeon to examine the inside of the joint, and cut, shave and remove material from the inside of the knee joint.
The Australian Orthopaedic Society does not recommend knee arthroscopies due to the lack of evidence showing any benefit. As an invasive procedure, arthroscopies also have the potential to cause more harm and pain.
Tips for daily activities and living well
There are many things you can do every day to manage your knee OA to minimise the effect it has on your life including:
- pacing – try to find the right balance between rest and activity. Aim to break up your chores into smaller tasks, and over a longer period of time, rather than all in one go. In between the smaller tasks, you can do activities that are less active or stressful on your sore knees. For example, if you’re vacuuming your house, break it into rooms. Vacuum one room, and then sit down and go through your mail, or write your shopping list. Then you can move on to the next room. If it helps, set a timer so you’re reminded to take a break.
- managing your pain – as well as exercise, weight loss (if needed) and short term use of medications, there are other things you can do to relieve your pain. Heat and cold packs can be quite soothing. Generally speaking, heat packs can help ease muscle pain and tension while cold packs can help with inflammation. When using heat or cold packs remember to wrap them in a cloth or towel so that they don’t directly touch your skin, as this can cause burns. For more tips on managing pain see our online book ‘Managing your pain – an A-Z Guide’.
- sleep – it’s important to get a good night’s sleep. If you wake with pain or discomfort during the night consider taking pain relieving medication before going to bed. Taking a warm bath before going to bed can also help you fall asleep. If you have difficulty getting in and out of a bath, try having a warm shower instead. Pillows between your knees (if you sleep on your side), hot water bottles or electric blankets can also be helpful when trying to get to sleep.
- aids and equipment – speak with an occupational therapist (OT) about assistive devices and aids such as canes/walking sticks, crutches and 4-wheel walkers. They can help to relieve the load on your knees and assist with balance. Some types of knee braces, taping and wedge shoe insoles, however, aren’t recommended for knee OA. It’s best to speak with your health professional to work out what’s suitable for you.
- kneeling – if you need to kneel for gardening, cleaning or other tasks, use a kneeling pad to help ease any discomfort from your knees – an old pillow wrapped in a plastic bag can do the job. You can also find knee pads that have handles that help you get down and up.
- suitable footwear – when trying to reduce the symptoms of knee OA it’s important to wear comfortable, well-fitted shoes. A flat shoe with a cushioned, flexible sole and a good arch support is often the best choice.
- shopping – get heavy shopping delivered if possible or ask a friend or family member for help.
- trip hazards – reduce the risk of falls at home by checking for any trip hazards e.g. uneven surfaces, rugs, electrical cords and cables etc.
- in the kitchen – use a trolley or other aids to move items around and prevent increasing the load on the knee/s when lifting heavy things. You could also use a stool to sit on when preparing food so you’re not having to stand for long periods.
- spread the load – always carry items close to the body and where possible divide items into smaller, easier loads. You don’t always need to carry everything in one go. And if you do, ask for help, or use a trolley.
- supportive chairs – try to use an armchair that isn’t too low; you shouldn’t struggle to get out of it and it shouldn’t cause you aches and pains when you’re sitting in it. It’s also helpful if your chair has sturdy arms to push up from and provides sufficient support when seated. If you’re thinking of buying a particular armchair, see if you can hire it so you can try before you buy.
- car modifications – a raised seat or a swivel seat may be helpful when getting in and out of the car – it may also help make driving more comfortable. When considering any additional car modifications/devices ensure that they’re professionally fitted for safety reasons. For further helpful tips when driving see our information about driving with a musculoskeletal condition.
- join a support group – people often find it very valuable to share experiences and recommendations with others in a similar situation. Search online or get in touch with your local arthritis office to see what support groups are near you.
Where to get help
- Your doctor
- Your physiotherapist
- Musculoskeletal Health Australia
Back Pain | Arthritis | Musculoskeletal Conditions (B.A.M) Helpline 1800 263 265 - GLA:D Australia treatment for hip and knee osteoarthritis https://gladaustralia.com.au/
How we can help
Call our Helpline and speak to our friendly team: phone 1800 263 265 or email helpline@muscha.org
We can help you find out more about:
- osteoarthritis and musculoskeletal conditions
- ways to live well with these conditions
- managing your pain
- read our A-Z guide to managing pain
- watch our excellent videos on pain, your brain and how you can retrain your pain system.
- Pain, the brain and your amazing protectometer – Lorimer Moseley
- Treating pain using the brain – David Butler
- upcoming webinars, seminars and other events.
More to explore
- My Knee Exercise mykneeexercise.org.au
- Better Health Channel betterhealth.vic.gov.au
- Australian Physiotherapy Association physiotherapy.asn.au
- Exercise and Sports Science Australia essa.org.au
- Australian Podiatry Association https://podiatry.org.au
- Occupational Therapy Australia otaus.com.au
- Dietitians Association of Australia http://daa.asn.au








