I think there’s a reason we respond so positively to the memes, social media posts and jokes that poke fun at pain, chronic illness and the trials and tribulations that come from living with both.
Having a foggy brain isn’t particularly funny, being unable to sleep isn’t a joke, and pain – wow, that’s probably the un-funniest thing you can think of 😣. But we all tend to laugh at and share the well-crafted meme or post that pokes fun at these things because we identify with the truth behind them. And with the best ones, you can tell it’s been created by someone who knows what it’s like to live with pain and illness. You recognise a fellow traveller.
Laughter and humour are such powerful forces. Just think about the last time you had one of those huge, spontaneous belly laughs with family or friends. Something was said, a joke was told, or you all saw something ridiculous. You snort, giggle, and guffaw. Your eyes water, you gasp for breath, and your belly starts to hurt. When you look at each other, you laugh some more. When you finally do stop laughing, you feel euphoric. Everything seems better, and you feel happier 😊.
However, when you’re in the grips of pain, laughing is probably the last thing you feel like doing. But laughter can actually help you deal with your pain better. A good joke, a funny movie, or just seeing something silly can distract you from your pain and make you feel better, at least for a while.
Laughter also causes your brain to release some feel-good chemicals that boost your mood and make you feel more optimistic. They include endorphins, serotonin and dopamine. Endorphins are your body’s natural pain reliever; releasing them into the body temporarily reduces your feelings of pain. Serotonin produces feelings of calmness and happiness. And dopamine is part of your brain’s reward system and gives you a sense of pleasure. It also helps reduce feelings of anxiety.
Other health benefits of a good giggle
As well as helping you cope with your pain and the stress of living with chronic health issues, laughter has many other health benefits. Laughing regularly:
- Is good for your lungs. It increases the amount of oxygen you breathe in, and if you do it often enough, it increases lung capacity by promoting deep breathing.
- Is good for your heart and improves blood pressure and circulation.
- Lifts your mood and provides relief from stress and anxiety.
- Is exercise! That’s why it’s often called ‘internal jogging’. 🏃🏃
- Decreases muscle tension.
- Helps you relax.
- Brings you closer to the people you’re laughing with.
- May improve immune function.
- Helps manage depression.
- Improves sleep quality.
- Is free! 😊
LOL ideas
To bring on the laughs, giggles, chortles, snickers, cackles and guffaws, give these ideas a go:
- Watch/stream a funny movie or sitcom – check out these lists from Flickchart and Rolling Stone for their top picks.
- Listen to a funny podcast – this list from Time Out will get you started if you need ideas.
- Run through a sprinkler on a hot day.
- Talk with a friend and reminisce about a funny experience you had together.
- Watch cat / dog / panda videos (you’re welcome!). 😹
- Grab the kids, friends, partner or housemates and play. Anything! … Keep a balloon off the floor. Throw a frisbee. Charades. Pub quizzes. Truth or dare. Never have I ever. The floor is lava…
- Have a pillow fight.
- Think about the funniest joke you ever heard or your best (worst) dad jokes.
- Jump on a trampoline.
- Take silly selfies and send them to your bestie.
- Grab a microphone (or a hairbrush) and sing out loud!
- Join a laughter club. Simply google ‘laughter clubs’ for your state or territory.
Sadly it’s not all fun and games
It’s important to remember that laughter and humour are temporary distractions from pain. They’re great, and we should definitely cram as much into our day as possible. Just for the sheer joy of it 🤡.
But when you have a chronic illness and persistent pain, a balanced treatment approach should include self-care, appropriate medications and medical care, a healthy lifestyle, exercise, mindfulness and, yes, laughter.
Laughter may not be the best medicine (as the old saying goes), but it’s pretty close to perfect.
So, make sure you take a dose (or better yet – several!) every day!
Contact our free national Help Line
Call our nurses if you have questions about managing your pain, musculoskeletal condition, treatment options, mental health issues, or accessing services. They’re available Monday to Thursday between 9am-5pm on 1800 263 265; email (helpline@muscha.org) or via Messenger.
More to explore
- How laughter works
HowStuffWorks - How laughter brings us together
The Greater Good Science Center at the University of California, Berkeley - How to use laughter to lift your mood
Happiful - Humor in psychology: Coping and laughing your woes away
PositivePsychology.com - Laughing is good for your mind and your body – here’s what the research shows
The Conversation - Laughter
Psychology Today - Laughter has serious benefits
Michigan State University - Laughter is the best medicine
Help.Guide.org - Mayo Mindfulness: Laughter for stress relief is no joke
Mayo Clinic - The health benefits of humor and laughter
Verywell Mind - The health benefits of laughter
Verywell Mind - Ways that humor can heal
PsychCentral
Photo by MI PHAM on Unsplash





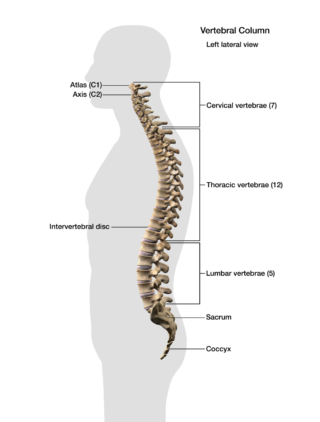 Let’s start with a look at your spine
Let’s start with a look at your spine












