In October 2022, the Albanese Government announced that they would invest almost $7 million in stem cell research. The ARISTOCRAT project, led by MSKs Director Emeritus, and orthopaedic surgeon Professor Peter Choong, will allow researchers to develop new therapies to improve the lives of people with conditions like osteoarthritis.
So what does this mean? What are stem cells? And, will they be the miracle treatment we’ve been waiting for?
Let’s take a look.
But first, what’s osteoarthritis?
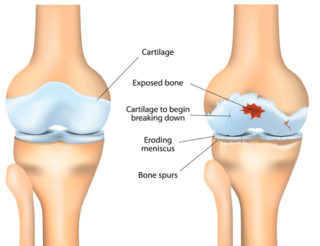
Osteoarthritis, or OA, is the most common form of arthritis. It most frequently affects the joints in the knees, hips, feet, spine and hands.
OA was once thought to be a natural part of ageing or a lifetime of ‘wear and tear’ on joints. But we now know it’s much more complex than that and may occur due to many factors.
With OA, the cartilage that lines the ends of bones in a joint, enabling them to move smoothly over each other, becomes brittle and breaks down. Because the cartilage no longer has a smooth surface, the joint becomes stiff and painful. Eventually, the cartilage can break down so much that it no longer cushions the two bones.
There are currently no treatments, including medicines, that can affect the underlying disease process of OA. Instead, symptoms (e.g. pain and stiffness) are managed using exercise, weight management and medicines that provide temporary relief.
The lack of targeted treatments to prevent OA from worsening or reversing the damage it causes makes the promise of new and innovative treatments, such as stem cells, very exciting.
So what are stem cells?
Cells are the basic building blocks of all living things. They provide structure for the body, take in nutrients from food, convert those nutrients into energy, and carry out specialised functions. Cells also contain the body’s hereditary material and can make copies of themselves. We have many different types of cells, such as nerve, bone, fat, blood, and stem cells.
Stem cells differ from other cells in the body in three ways:
- they can divide and renew themselves over a long time
- they’re unspecialised, so they can’t do specific functions in the body
- they can become specialised cells, such as muscle cells, blood cells, and brain cells.
There are many types of stem cells. However, the type of stem cell most often promoted as a treatment for osteoarthritis is the mesenchymal stem cell or stromal cell. They’re generally referred to as MSCs (because no one can say mesenchymal 😉). These cells can be obtained from many parts of the body, including bone marrow and fat.
MSCs can become bone cells (osteoblasts), cartilage cells (chondrocytes), muscle cells (myocytes), or fat cells (adipocytes). They can also release substances that may alter how the immune system responds to injury and encourage other cells to grow.
This has led scientists and doctors to explore whether MSCs can restore function to damaged joints and tendons.
EuroStemCell has an interesting article that explains MSCs – what they are, what researchers are investigating when it comes to MSCs, and the challenges they face.
More research is needed
For most conditions, stem cell treatments are still considered experimental. They have yet to prove safe or effective in clinical trials for osteoarthritis.
While there’s a lot of excitement about the future, we need more research to understand how to best obtain, handle and administer stem cells or the cells made from them.
We need to know some of these answers to ensure that new stem cell treatments don’t cause more harm than good.
We also need more information about potential side effects and the long-term safety of stem cell treatments.
Be wary
Unfortunately, despite the lack of reliable evidence that stem cell treatments work and are safe to use, they’re actively promoted for osteoarthritis and many other health conditions by clinics in Australia and overseas.
Some clinics use cells obtained from the person on the same day they’re collected, while others may grow the person’s or donor cells in the lab over several weeks before returning them to the person. It’s important to know that even when the cells are taken from a person and returned to the same person, there’s still risk involved. Even though they’re your own cells, the fact that they’ve been removed means there’s the risk that they may have become contaminated.
Most clinics charge substantial fees (thousands of dollars). They encourage multiple treatments and may imply they’re doing research but aren’t usually part of a registered clinical trial. They also often use celebrity patients’ testimonials or endorsements to support their claims of success.
That’s why participating in a clinical trial is currently the safest way to access stem cell treatments. Researchers must follow strict rules to ensure that participants are safe. Each clinical trial also follows a careful study plan or protocol that describes what the researchers will do.
Before joining a clinical trial, you’ll be told what to expect as a participant and all the things that might happen. For example, someone from the research team will explain possible side effects or other risks of the treatment. You’ll also have a chance to ask questions about the trial. In most cases, you won’t be required to pay any costs involved in participating in a clinical trial. There may be out-of-pocket expenses, such as travel, which may be reimbursed to you.
Ask questions
If you’re considering trying a stem cell treatment, you need to be well-informed – so ask lots of questions. For example:
- Is this treatment part of a registered clinical trial listed on the Australian New Zealand Clinical Trial Registry (ANZCTR), ClinicalTrials.gov, or elsewhere?
- Was ethics review and approval obtained, and by whom?
Note – All clinical research projects in Australia must be approved by a Human Research Ethics Committee (HREC), which checks that the research conforms to the National Statement on Ethical Conduct in Human Research requirements. - Does the doctor, or any of the researchers involved, have any conflicts of interest, including financial?
- What are the total costs of the treatment, and how much will I be expected to pay? Remember, if you’re taking part in a clinical trial, no costs should be involved.
- Will you use my own cells, or are they from a donor or other source?
- How does this treatment compare to other treatments?
- Is there any scientific evidence (not testimonials or anecdotes) that the treatment improves my health condition?
- What are the potential side effects or risks involved?
- How many treatments are required?
- How long do you monitor the effects of my treatment?
Stem cell treatments are still considered experimental for osteoarthritis, so don’t be embarrassed to ask lots of questions. Learn as much as possible about the treatment and how it might affect you. You should also have a chat with doctor or specialist about your intentions and get their input.
Stem cells and cell therapy are an exciting new frontier in medicine, but it’s still early days. So watch this space.
And watch our video, Stem cells and muscle, bone and joint health: Hope, hype and reality, presented by Professor Megan Munsie, Deputy Director – Centre for Stem Cell Systems, The University of Melbourne; Head – Education, Ethics, Law & Community Awareness Unit, Stem Cells Australia.
Contact our free national Help Line
Call our nurses if you have questions about managing your pain, musculoskeletal condition, treatment options, mental health issues, telehealth, or accessing services. They’re available weekdays between 9am-5pm on 1800 263 265; email (helpline@msk.org.au) or via Messenger.
More to explore
- 5 things you should know about stem cells
Australasian College of Sport and Exercise Physicians - Australia first stem cell research to help adults and children living with joint pain and disfigurement
Department of Health and Aged Care - MSCs: the ‘other’ bone marrow stem cells
EuroStemCell - Nine things to know about stem cell treatments
International Society of Stem Cell Research - Osteoarthritis
Stem Cells Australia - Stem cells and muscle, bone and joint health: Hope, hype and reality
Musculoskeletal Australia - Stem cells
healthdirect - What is a clinical trial?
Commonwealth Department of Health and Aged Care - What is a stem cell?
yourgenome