Most people think that arthritis only affects older people, but children can get it too. It’s estimated that between 1 in 800 and 1 in 1,000 children in Australia have arthritis.
What is juvenile idiopathic arthritis (JIA)?
JIA is a group of inflammatory conditions that cause joint pain and swelling in children and teens under 16.
What causes JIA?
We don’t really know what causes JIA. That’s what ‘idiopathic’ means, ‘from an unknown cause’.
But we do know it occurs due to a malfunctioning immune system.
The job of your immune system is to look out for and attack foreign bodies – like bacteria and viruses – that can make you sick. However, in the case of JIA, the immune system mistakenly targets healthy tissue in and around the joints, causing ongoing inflammation and pain. We don’t know why this happens, but scientists believe that a complex mix of genes and environmental factors is involved.
Types of JIA
There are several types of JIA, each with distinct features.
Oligoarthritis JIA
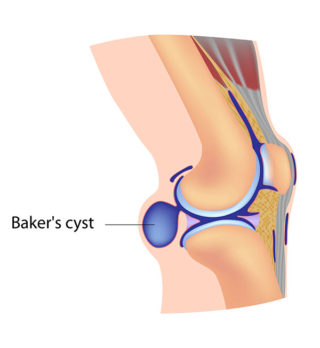
This is the most common type of JIA. It’s also called oligoarticular or pauciarticular JIA. Both ‘oligo’ and ‘pauci’ mean not many or few. Less than five joints are typically affected, most commonly one or both knees. Children with oligoarthritis may also develop inflammation of the eye, called uveitis.
Polyarthritis JIA
Polyarthritis (or polyarticular) JIA affects five or more joints. ‘Poly’ means many. It often affects the joints in the fingers, toes, wrists, ankles, hips, knees, neck and jaw.
There are two types of polyarthritis JIA, based on whether rheumatoid factor (proteins produced by the immune system) are found in the blood. They are polyarthritis JIA (rheumatoid factor positive) and polyarthritis JIA (rheumatoid factor negative).
Enthesitis-related JIA
Entheses are the tissues that attach tendons and ligaments to the bone. Enthesitis-related JIA causes inflammation and pain in the entheses (enthesitis) and joints (arthritis). The most common locations for enthesitis are the knees, heels, and bottoms of the feet. Arthritis is generally in the hips, knees, ankles, feet, and spine.
Psoriatic JIA
Children with psoriatic arthritis have inflammatory arthritis of the joints and the skin condition psoriasis. It often affects the fingers and toes, but other joints can be affected. It can also cause pitted fingernails and swollen fingers or toes.
Systemic JIA
Systemic JIA can affect many areas of the body, not just the joints. It usually starts with fever and rash that come and go over a period of weeks. It’s the least common type of JIA.
Undifferentiated JIA
This is where the condition doesn’t fit any of the above types of JIA.
What are the signs that my child may have JIA?
The signs or symptoms of JIA vary depending on the type of arthritis a child has. Some of the more common symptoms include:
- Pain, swelling and stiffness in one or more joints
- The skin over the affected joints may be red or warm
- Mental and physical tiredness (fatigue).
Less common symptoms include:
- Fever
- Rash
- Feeling generally unwell
- Eye inflammation (uveitis).
The symptoms of JIA vary from child to child and are likely to change as they get older.
At times, symptoms can become more intense; this is a flare. Flares can be unpredictable and often seem to come out of nowhere.
There may also be times when your child experiences a remission – where their symptoms go away for a time.
What is uveitis?
Uveitis is inflammation of parts of the eye. It’s also the result of a malfunctioning immune system.
The most common type of uveitis has no symptoms (sometimes called silent uveitis). This means that it doesn’t hurt, and you won’t be able to tell if your child has uveitis just by looking at their eyes. Some children do have symptoms such as blurred vision, light sensitivity, and in rare cases, eye redness and pain.
If uveitis isn’t treated, it can cause permanent vision loss. This means that all children with JIA need regular check-ups with an ophthalmologist (specialist eye doctor) to check for uveitis and start treatment if needed.
How is JIA diagnosed?
JIA can be challenging to diagnose because the symptoms differ between children, and many symptoms are similar to those experienced with other illnesses.
There isn’t one single test that can be used to diagnose JIA, and your doctor will usually use a combination of tests to confirm your child’s diagnosis, including:
- a physical examination to assess joint tenderness, flexibility, and stiffness
- blood tests to check for inflammation associated with JIA, which can also help to work out which type of JIA your child has
- scans such as x-ray and MRI (magnetic resonance imaging) to check for joint inflammation and damage
- an eye examination.
If you visit your family doctor (GP) and your child has symptoms that suggest it might be JIA, they’ll usually order some of these tests and refer you to a doctor who specialises in juvenile idiopathic arthritis, called a paediatric rheumatologist. Seeing a rheumatologist as soon as possible is essential to ensure your child gets the best outcomes.
How is JIA treated?
While there’s no cure for JIA, there are many treatments to help manage the condition and its symptoms so your child can continue to lead a healthy and active life. Because every child’s experience of JIA is different, treatment will be tailored to best meet your child’s needs.
Finding the right combination of treatments may take time and is likely to change as the JIA symptoms change or your child grows.
For most children and young people, treatment will include exercises to keep joints moving and muscles strong, medicines to reduce inflammation, splints to support joints, and pain management strategies.
Medicines
Most children with JIA – regardless of the type – will need to take some form of medicine at some time. The medicines that your rheumatologist prescribes for your child will depend on their symptoms, including how much pain and inflammation they have.
There are many different types of medicines that work in different ways. The main types of medicines used to treat JIA and help manage its symptoms include:
- Analgesics (or pain relievers) provide temporary pain relief. They can range in strength from mild to very strong. You can buy many of them over the counter at your pharmacy or supermarket. However, stronger medicines, including those containing codeine, require a prescription.
- Creams and ointments (also called topical analgesics and anti-inflammatories) applied to the skin over a painful joint can provide temporary pain relief.
- Non-steroidal anti-inflammatories (NSAIDs) also provide temporary pain relief, specifically pain associated with inflammation. You can buy some over-the-counter, but stronger NSAIDs require a prescription.
- Corticosteroids act quickly to control or reduce inflammation, pain and stiffness. They can be taken in tablet form, or may be given as an injection into a joint, or from a drip into a vein.
- Disease-modifying anti-rheumatic drugs (DMARDs) control your child’s overactive immune system. They help relieve pain and inflammation and reduce or prevent joint damage.
- Biological disease-modifying medicines (bDMARDs, or biologics and biosimilars.) also work to control the immune system. However, unlike other disease-modifying drugs, biologics and biosimilars target the specific cells and proteins that cause inflammation and tissue damage rather than suppressing your entire immune system.
- Eye drops to treat eye inflammation (uveitis).
What can we do to control symptoms?
As well as taking any medicines as prescribed, things you and your child can do to manage JIA include:
- Learning about JIA. Understanding the condition and how it affects your child means you can make informed decisions about their healthcare and actively manage it.
- Following the treatment plan that your health professionals have developed. That means taking medicines as prescribed, doing the exercises the physiotherapist and/or occupational therapist have provided, and letting your doctor know of any changes to your child’s symptoms and how they’re feeling. All these things give your child a better chance of managing their JIA well and reducing the risk of long-term problems.
- Staying active. Regular exercise is the key to maintaining muscle strength, joint flexibility and managing pain. A physiotherapist or exercise physiologist can help design an individual program for your child.
- Learning ways to manage pain. There are many ways your child can manage pain from heat and cold treatments, distraction, massage and medicine. Try different techniques until you find the things that work best for your child.
- Eating a healthy, balanced diet. While no diet can cure JIA, a healthy diet is the best for good health, especially for growing children. Keeping to a healthy weight is also important as extra weight strains your child’s joints, especially load-bearing joints such as hips, knees and ankles.
- Protecting the joints. Aids, equipment, and gadgets can make activities easier for your child. They include an ergonomic mouse and keyboard for your child’s computer, a supportive chair or back support cushion, and foam rubber to make pencils, pens, brushes, and cutlery handles easier to grip. An occupational therapist (OT) can advise you on available equipment and techniques to reduce strain on joints from everyday school activities.
- Using splints. Splints are commonly used as a treatment for JIA, particularly for wrists and feet. They’re used to rest or support sore or inflamed joints, stretch out a joint, and help make some activities easier.
- Staying at school. This is essential for your child’s health and wellbeing, as well as their education and socialisation. Talk with your doctor, allied health professionals and teachers about ways to help your child stay at school and keep up with school.
Contact our free national Help Line
Call our nurses if you have questions about managing your pain, musculoskeletal condition, treatment options, mental health issues, COVID-19, telehealth, or accessing services. They’re available weekdays between 9am-5pm on 1800 263 265; email (helpline@msk.org.au) or via Messenger.
MSK Kids
Our free MSK Kids program provides a range of programs and services along with evidence-based information and resources for children living with juvenile arthritis (JIA) and other musculoskeletal conditions. Resources are available for the child, family and school. Find out more about MSK Kids.
More to explore
- Juvenile arthritis (JA)
Arthritis Foundation - Juvenile Arthritis
American Academy of Orthopaedic Surgeons - Juvenile arthritis
American College of Rheumatology - Juvenile Idiopathic Arthritis (JIA)
National Institute of Arthritis and Musculoskeletal and Skin Diseases - Juvenile idiopathic arthritis (JIA)
Versus Arthritis - Resource Hub
JIA-at-NRAS (National Rheumatoid Arthritis Society)