Do you remember the TV show House? Hugh Laurie played the brilliant but grumpy, antisocial doctor addicted to pain meds who secretly has a heart of gold. Yep, it had all the cliches. 😂.
The show created a lupus meme – where a diagnosis of lupus was often mentioned on the show to which House’s reply would always be, ‘it’s not lupus’. And most of the time, he was right.
The meme highlights that lupus is rare, complex, and difficult to diagnose.
And sometimes, it is lupus (as was the case in an episode in season 4).
So what is lupus?
Lupus (systemic lupus erythematosus) is a chronic condition that can cause inflammation and pain in any part of your body. Symptoms vary from person to person and can range from mild to severe.
Anyone can get lupus; however, women are more likely to develop it than men. It’s usually diagnosed in people aged between 15-45.
Certain ethnic groups are also more likely to develop lupus, such as Indigenous Australians, Africans, Hispanics, Asians and Native Americans.
Causes
Lupus is an autoimmune disease. That means it occurs as a result of a faulty immune system.
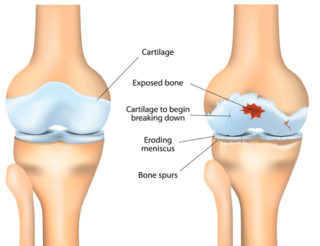
Your immune system is designed to identify foreign bodies (e.g. bacteria, viruses) and attack them to keep you healthy. But in the case of lupus, your immune system mistakenly targets healthy tissue.
This causes pain and inflammation in parts of the body such as the skin, joints, and internal organs (e.g. kidneys, heart and lungs).
We don’t know why this happens. Scientists believe a complex mix of genes and environmental factors may be involved.
Symptoms
Symptoms can vary greatly between people and may include:
- skin rashes
- joint and muscle pain
- sensitivity to light
- hair loss
- fatigue
- fever
- mouth ulcers
- weight changes
- organ involvement (e.g. kidneys, heart, lungs)
- pale, blue, or red fingers or toes triggered by cold or stress (Raynaud’s phenomenon)
It’s unlikely that one person will experience all of these symptoms. At times the symptoms you experience due to your lupus (e.g. rash, pain, fatigue) will become more intense. This is a flare.
Flares are unpredictable and can seem to come out of nowhere. They’re often triggered by stress or exposure to ultraviolet light.
Diagnosis
Lupus can be a difficult condition to diagnose. Symptoms vary significantly from one person to another and are similar to those of other conditions. They can also change or fluctuate. So, it may take months or years to get a definitive diagnosis of lupus.
No single test can diagnose lupus, so your doctor will use a combination of tests to confirm your diagnosis. They may include:
- Your medical history. Your doctor will ask about your symptoms, family history and other health issues.
- A physical examination – including your joints and skin to look for any signs of change, inflammation and rashes.
- Blood and urine tests.
- Tissue biopsies of the skin or kidneys.
Test results also help rule out other conditions that may have similar symptoms.
Your GP should refer you to a rheumatologist if they think you have lupus. Rheumatologists are doctors who specialise in diagnosing and treating problems with joints, muscles, bones and the immune system.
Treatments
While there’s no cure for lupus, treatments are available to help control disease activity and improve symptoms. They include medicines and self-care.
Medicines
Medicine can help manage your symptoms and assist in controlling your immune system.
Because people with lupus experience different symptoms, and to varying degrees, there’s no ‘one size fits all’ treatment. You might need to take a combination of medicines.
- Hydroxychloroquine is very effective at reducing inflammation and reducing flares. It’s the first-line medicine for most people with lupus.
- Non-steroidal anti-inflammatory drugs or NSAIDs may temporarily relieve pain and inflammation. NSAIDS should be avoided by people with kidney disease.
- Corticosteroids (or steroids) are used to quickly control or reduce inflammation. They come in different forms: tablets, injections, or a cream to apply to skin rashes.
- Disease-modifying drugs may be needed to suppress your immune system and control symptoms if you don’t respond to hydroxychloroquine and/or steroids.
- Biological disease-modifying medicines (biologics and biosimilars) also suppress the immune system. They may be used in more severe cases of lupus that aren’t responding to treatment. These medicines target the specific cells and proteins that cause inflammation and tissue damage rather than suppressing your entire immune system.
All medicines can have side effects. It’s important you discuss these with your doctor and know what to do if you experience any. Your doctor will also monitor your response to the medicines closely. You may need regular blood tests depending on the medicines you’re taking.
You should also inform your doctor of any other medicines or complementary therapies you take. They can potentially affect your lupus medicines.
Self-care
There are many things you can do to manage your lupus.
- Learn about your condition. Understanding lupus allows you to make informed decisions about your healthcare and actively manage it.
- Manage your exposure to ultraviolet (UV) light. UV light, especially sunlight, can cause a flare. This can include skin rashes in sun-exposed areas. Remember to wear 50+ UVA and B sunscreen daily (even if it’s cloudy). You should also cover your skin and wear a hat and sunglasses outdoors. Less commonly, UV light from fluorescent lights, including low-energy light bulbs, may cause rashes in some people with lupus.
- Stay active. Regular physical activity has many health benefits, including helping you to manage your symptoms. When you start exercising regularly, you should notice an improvement in the quality of your sleep, an increase in energy levels, a reduction in fatigue, and improvements in your overall strength and fitness. Exercise can also help prevent long-term consequences of lupus, such as heart disease and osteoporosis.
- Learn ways to manage your pain. Pain is one of the most common symptoms of lupus, so it’s crucial to learn ways to manage it effectively. Read our A-Z guide for managing pain for more information.
- Manage stress. Stress can aggravate your symptoms, so learning to deal with stress is very helpful. Things you can do to manage stress include planning your day and setting priorities, using relaxation techniques, getting a massage or listening to music. And, where possible, avoiding people and situations that cause you stress.
- Quit smoking. Smoking cigarettes can worsen your lupus symptoms and reduce the effectiveness of particular lupus medicines. It can also affect your bone health and increase inflammation.
- Ask your GP about your vitamin D, calcium and cholesterol levels. Lupus can affect them all, and you may need to take supplements or medicines to correct any problems.
- Sleep well. Not getting enough quality sleep can worsen your symptoms; however, getting a good night’s sleep when you have chronic pain can be difficult. If you’re having problems sleeping, talk with your doctor about how you can address this.
- Eat a healthy, balanced diet. While there’s no specific diet for lupus, it’s important to have a healthy, balanced diet to maintain general good health and prevent other health problems, such as diabetes and heart disease. Lupus can also cause weight loss or gain depending on how it affects your body and the medicines you take. A healthy balanced diet may help prevent this. Talk with your doctor if you’re concerned about your diet or weight.
- Pace yourself. Pacing is an effective strategy to help you do the things you want to do by finding the right balance between rest and activity (both physical and mental). This will help reduce your risk of flares and fatigue.
- Get support from others. Research has shown that people with positive social support cope better with pain. Family, friends, colleagues, and health professionals can help you manage. A peer support group may be another option.
Pregnancy
Most women with lupus can have children. However, there’s an increased risk of complications such as premature labour, high blood pressure, blood clots and miscarriage.
For these reasons, you must plan your pregnancy carefully.
The healthier you are before you get pregnant, the greater the chance you’ll have a healthy pregnancy and baby. Aim to have your condition under control and be in the best possible health.
Talk with your doctor and specialist before you get pregnant. They may need to change your medicines to ensure a safe pregnancy.
Complications
Lupus is an unpredictable condition that can affect any part of your body, including your internal organs. Working closely with your healthcare team, following your treatment plan, and staying informed about lupus is the best thing you can do to reduce your risk of complications.
Contact our free national Help Line
Call our team if you have questions about managing your pain, musculoskeletal condition, treatment options, mental health issues, telehealth, or accessing services. They’re available weekdays between 9am-5pm on 1800 263 265; email (helpline@muscha.org) or via Messenger.
More to explore
- Lupus
American College of Rheumatology - Lupus
Healthdirect - Lupus (SLE)
Versus Arthritis - Lupus Foundation of America
- Lupus UK
- Patient education: Systemic lupus erythematosus (Beyond the Basics)
UpToDate