Tips to help you sweep away winter
Spring is such a wonderful time of year 😊🌼. The mornings are becoming lighter, the weather’s improving, and the smell of spring blossoms is in the air. So take a moment to breathe it in – you’ll definitely feel a lift in your mood (unless you have allergies – sorry about that 🤧).
It’s also the perfect time to do a bit of spring cleaning; of your home, office, garden or garage. Especially if, like me, you open the blinds on a sunny day and the sunlight highlights every dust bunny, dirty surface, and pet hair tumbleweed 😮.
But cleaning and reorganising can take a toll when you live with a musculoskeletal condition, chronic pain, and fatigue. So we’ve got some tips to help you clean without overdoing it.
Planning, prioritising and pacing
First, make a plan. You can’t do everything at once. So write down all of the things you want to do.
Now prioritise the jobs. What’s most important? And when you consider this, remember your home doesn’t need to be a glossy magazine or Pinterest version of ‘perfect’. That takes a lot of styling, filters, and constant effort. It just needs to be your version of ‘perfect’ – comfortable and cosy for you and whoever you live with.
And finally, pacing. Take your time when you tackle your cleaning. Break it into smaller tasks. For example, don’t try to organise and clean your entire bedroom cupboard in one go. Go small. Deal with your shoes one day; the next day, you can focus on the things stored on shelves, and so on. Make it achievable and realistic for you and how you’re feeling.
Take breaks
We’re often tempted to get as much done as possible while we’re feeling good or motivated. But you need to take breaks so that you don’t overdo it. Otherwise, before you know it, your back’s sore, you can’t move your neck, and exhaustion hits you like a sledgehammer.
Set an alert on your phone to prevent this from happening. Give yourself a specific time to work and take a break when the alert chimes. Do some stretches, drink water, go outside for some air and vitamin D, or have a healthy snack if you’re hungry.
And if you find yourself getting tired, or starting to ache before the alert goes off, listen to your body readjust your timing, and take an earlier break.
Taking regular breaks, rather than pushing through, will leave you feeling much better at the end of your cleaning session.
Get the right tools for the jobs
Lightweight brooms, mops and vacuums make life much easier, especially if you have stairs or a large space to clean. Upright or robotic vacuums can be helpful as you don’t need to bend over a lot, especially when compared with barrel vacs. Just be aware of where the robots are so you don’t trip over them 😐!
Use an upright dustpan to sweep up crumbs, fluff and other debris from the floor. They require minimal bending, which is great if you have a sore back or get dizzy when you bend over.
Long-handled dusters can help you reach high places, especially if stretching or reaching your arms above your head is painful. If you don’t have one, you can attach your duster to a piece of dowel or a ruler to give you the extra length. Or even better, get someone else to do the dusting!
And don’t forget to use your reacher, grabber or other pick-up tools if you have one. They’re not just handy for retrieving something you’ve dropped but also for cleaning. You can pick up stray toys, socks and other items from the floor and retrieve light objects from high shelves.
Choose your battles
If you need to vacuum but aren’t up to doing your entire home, don’t. Just do the high-traffic areas. Or a high-traffic area. If your bathroom needs cleaning, do the high-use areas. Your shower screen doesn’t need to sparkle, but you do need clean towels and a clean sink.
Let the cleaning products do the hard work
Have you ever read the instructions on your cleaning products? Or do you just spray and wipe away? I’m definitely guilty of that! But many cleaning products need time to work on the grunge and grime. Then you can wipe it and the dirt away with far less effort. It’s also good to know that you don’t need separate multipurpose, kitchen and bathroom sprays. Choice has tested many of these products and found that they basically work the same. So you can save your money and cupboard space and just buy one.
Beware of dust and toxic smells
Many people with musculoskeletal and other chronic conditions are sensitive to chemicals, strong smells and/or dust. Some alternatives to the usual cleaning products include bi-carb soda, vinegar, tea tree oil, lemon juice and water. Many websites provide details for making your own cleaning products. There’s also a large range of more natural and plant-based cleaning products you can buy online and from the supermarket.
As far as dust goes, dusters often just move it from your surfaces to the air around you. Use a slightly damp cloth over surfaces to remove dust, and rinse it frequently. Or use an electrostatic duster that attracts and holds onto the dust.
Recycle old socks
I’ve recently discovered that old socks are perfect for many cleaning jobs around the house. You can put one on your hand and wipe down furniture, clean skirting boards, shutters, blinds, ceiling fans and even your indoor plants. When you’ve finished, you can remove the sock from your hand by pulling it off inside-out, and the dust and grime stay off your hand.
You can also put some potpourri or lavender into a sock, tie or sew the end shut, and stick it in the back of your closet, drawers, and other closed-up spaces you want to freshen up. 😊🌸🌻🌼🌷
Use your dishwasher for more than dishes
Did you know you can clean plastic toys, thongs, metal keys, exhaust covers, scrubbing brushes, and even dog toys in your dishwasher? Check out this article: Can you wash it in the dishwasher? The big list of things you can and can’t wash in the dishwasher from Choice for more info.
Consider reorganising your pantry, laundry or kitchen
These are the areas we use a lot. And they often have heavy things we use regularly – e.g. packets of rice, canned goods, pots and pans, detergents and cleaning products. Put these heavy items at waist level (if you have the space) so you aren’t constantly bending or stretching to access them. Check out Pinterest for ideas and inspo.
Get some wheels
A basket of wet washing or a bucket full of water can be really heavy. Instead, use a laundry trolley or a mop bucket with wheels.
Repackage it
We often buy cleaning products in bulk as it tends to be cheaper. But that can end up being several kilos or litres. So when you buy a big box or bottle of cleaning products, put a quantity into smaller, easier-to-use containers. You can top them up when you need to. And make sure you label the new containers clearly.
Alternate your cleaning activities
If you’ve spent some time doing physically tiring cleaning, take a break and do something more passive, like sitting at your desk and cleaning out your email inbox or reviewing receipts for your tax return. Or take a break and read a book or do some guided imagery. Then when/if you feel up to more physical work, you can go back to it. The important thing is you’ve given your body a chance to rest.
Get the family involved
This is obvious, but often such a drama that many of us just end up doing the chores ourselves 😑. But that’s not sustainable. Also, as everyone contributes to the mess, everyone needs to contribute to the cleaning. Read ‘How to divide chores around the home and get kids involved’ from RACV for some tips.
De-clutter
When we have a build-up of clutter and everyday things invading our space, they can become a trip hazard. Here are some ways to tackle the mess.
- Make a plan and start small.
- Organise the clutter by putting ‘like’ things together. For example, in your linen cupboard, put all your towels together in one group, bedsheets in another etc.
- Decide what you want to keep and what’s just taking up valuable space. Then you need to decide what to do with the things you no longer want. So donate, give away, sell, and repurpose what you can. Or if it’s damaged/worn out/soiled/beyond repair, recycle or throw it away.
Hire someone
This isn’t an option for everyone or for every time, but there might be occasions you decide it’s worth the cost. Consider hiring a local handyperson/business to help with your lawns/gardening or cleaning your carpets, curtains or blinds.
Distract yourself with music, podcasts and audiobooks
This can make the cleaning more enjoyable. Just be mindful of the passing time, so you don’t get distracted and overdo things 😉.
Give your medicine cabinet a spring clean too
Get rid of out-of-date or unnecessary items. But don’t throw medications in the bin – take them to your local pharmacy for disposal.
Things don’t have to be perfect…
So give yourself a break. As a clean freak, I constantly struggle with this. But listening to your body and doing things that are realistic for you is more important than some idea of perfection that’s unsustainable (or unattainable). Accept that and just enjoy being in your home 😊.
Call our Help Line
Call our nurses if you have questions about managing your pain, musculoskeletal condition, treatment options, mental health issues, telehealth, or accessing services. They’re available weekdays between 9am-5pm on 1800 263 265; email (helpline@msk.org.au) or via Messenger.
More to explore
- 15 cleaning games that make even the most boring chores fun
Mumtastic - 20 helpful tips for cleaning and organising when you’re chronically ill
Fed Up with Fatigue - 26 ‘hacks’ that can make cleaning easier if you have a chronic illness
The Mighty - Day by day: Cleaning with a chronic illness
Waking Up Amy - How to get rid of pet hair at home: Handy tips on how to keep the hairy onslaught to a minimum.
Choice - Spring clean checklist: Your room-by-room checklist for preparing your home for the warmer months
Choice



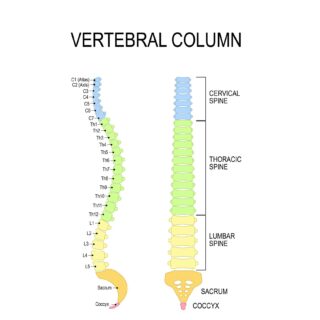 Let’s start with a look at your spine
Let’s start with a look at your spine