What do Lucille Ball, Kathleen Turner, Caroline Wozniacki, Pierre-Auguste Renoir, Edith Piaf, James Coburn and more than 450,000 Aussies have in common?
They all live (or lived) with rheumatoid arthritis (RA).
So, what is RA?
Rheumatoid arthritis is a type of inflammatory arthritis that causes pain, swelling and stiffness in the joints.
The most commonly affected joints are in the hands, feet and wrists.
What causes it?
Rheumatoid arthritis is an autoimmune disease. That means it occurs as a result of a faulty immune system.
Your immune system is designed to look out for and attack foreign bodies – like bacteria and viruses – that can make you sick. For reasons we don’t fully understand, when you have RA, your immune system gets confused. It targets your joints and healthy tissues as if they were foreign bodies. This causes ongoing inflammation and pain.
We don’t know why this happens, but scientists believe a complex mix of genes and environmental factors, including smoking, is involved.
What does RA do?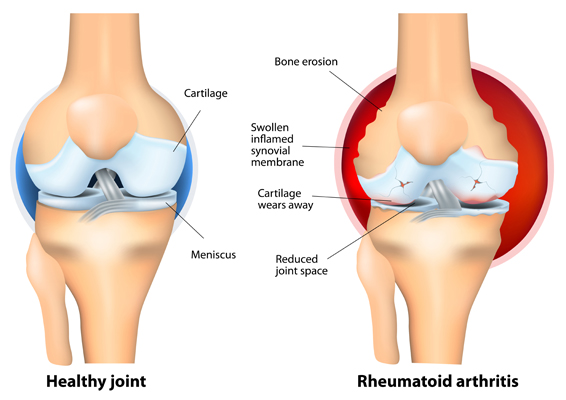
To understand how RA affects your body, it’s helpful to know a little about your joints.
Joints are places where bones meet. Bones, muscles, ligaments and tendons work together so you can twist, bend and move about.
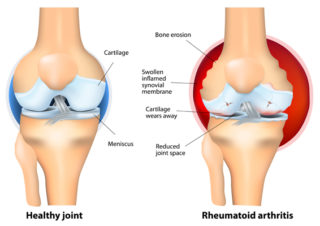
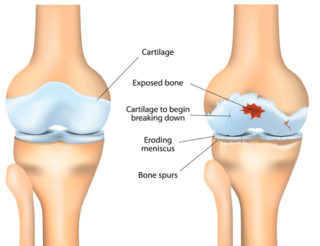
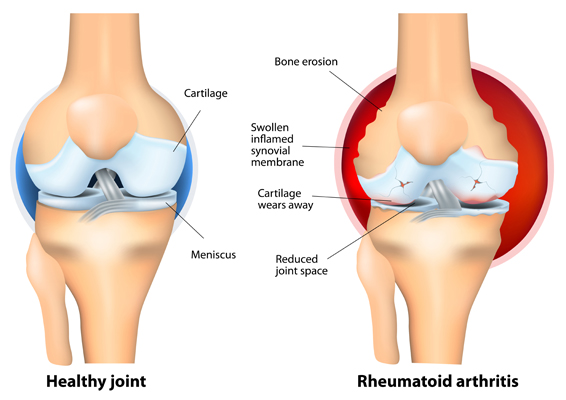
The ends of your bones are covered in a thin layer of cartilage. It acts like a slippery cushion absorbing shock and helping your joint move smoothly.
The joint is wrapped inside a tough capsule filled with synovial fluid. This fluid lubricates and nourishes the cartilage and other structures in the joint.
When you have RA, and the immune system targets your joints, it causes a build-up of synovial fluid and inflammation of the tissues that line the joint (synovial membrane). This causes pain, heat and swelling.
Cartilage becomes brittle and breaks down. Because the cartilage no longer has a smooth surface, the joint becomes stiff and painful.
Ligaments, tendons and muscles surrounding the joint can also be affected, causing joints to become unstable.
What are the symptoms?
The most common symptoms of RA include:
- joint pain
- joint swelling, heat and redness
- joint stiffness, especially in the morning or after sitting or being inactive for a while
- fatigue, or tiredness that doesn’t go away, even after sleeping or resting.
RA can affect any joints in the body, but most often affects the small joints in your hands and feet first.
Usually, the same joints on both sides of your body are affected – but this doesn’t always happen.
Other symptoms of RA can include:
- fleshy lumps called rheumatoid nodules; they form under the skin around affected joints and at places where your bones are close to the skin (e.g. elbows)
- dry eyes
- fever
- short-term interruption of blood flow to your extremities (e.g. fingers and toes), called Raynaud’s phenomenon.
RA can affect other parts of your body, including the eyes, heart and lungs.
Anyone can develop RA, but it most often appears in people aged between 30 and 60. It affects women more often than men. However, when women reach menopause, the incidence of RA becomes about the same for men and women.
How RA develops, and its severity will differ for each person. Symptoms can develop gradually or can start with a sudden, severe attack. Your symptoms can change daily, and they can sometimes become much worse. This is called a flare or flare-up. At other times, your symptoms may go away. This is called remission.
How is it diagnosed?
If you’re experiencing joint pain and inflammation, discussing your symptoms with your doctor is important. Many things can cause joint pain and swelling, including injuries, infection, and arthritis.
Getting a diagnosis as soon as possible means that treatment can start quickly. Early treatment will help you to control the inflammation, manage pain more effectively and minimise the risk of long-term joint damage and disability.
No single test can diagnose RA, so your doctor will use a combination of tests to confirm your diagnosis. They may include:
- Your medical history. Your doctor will ask about your symptoms, family history and other health issues.
- A physical examination to assess joint tenderness, flexibility, and stiffness.
- Blood tests to check for inflammation and antibodies associated with RA.
Scans such as an x-ray or MRI (magnetic resonance imaging) may be used to exclude other conditions or to look for joint inflammation or damage.
Your GP will refer you to a rheumatologist if they think you have RA. Rheumatologists are doctors who specialise in diagnosing and treating problems with joints, muscles, bones and the immune system.
How is RA treated?
While there’s no cure for RA, there are many treatments to help you manage the condition and its symptoms so you can continue to lead a healthy and active life. The ultimate goal is to reach a stage where you have very low or no disease activity – or remission. This can take trial and error, but some people can achieve remission or low disease activity once they start treatment.
Medicines
Your rheumatologist will recommend and prescribe medicines for your RA. Most people need to take more than one medicine because different medicines work differently.
The types of medicines used to treat RA and manage its symptoms include:
- disease-modifying anti-rheumatic drugs (DMARDs), which reduce the activity of your immune system. There are different categories of DMARD:
- conventional synthetic DMARDs or csDMARDs – e.g. methotrexate. Your rheumatologist will prescribe one of these medicines when you’re first diagnosed. They’ve been used for many years to treat RA and are very effective for most people. They’re called first-line medicine because they’re tried first. They may be used on their own or along with other DMARDs.
- biological DMARDs or bDMARDs – e.g. adalimumab. bDMARDs are used if the csDMARD hasn’t worked well enough to control your RA or stops working. They’re called second-line medicines.
- targeted synthetic DMARDs (tsDMARDS) – e.g. tofacitinib. They’re also a second-line medicine.
All DMARDs reduce the activity of your overactive immune system; however, the biological and targeted synthetic DMARDs are both more targeted to specific immune cells or processes.
- corticosteroids (or steroids) – e.g. prednisolone, act quickly to control or reduce inflammation and may be used in the short-term while you’re waiting for the DMARDs to take effect. They aren’t used for long periods as they’re associated with serious side effects.
- pain relievers (also called analgesics) for temporary pain relief
- non-steroidal anti-inflammatories drugs (NSAIDs) for temporary pain relief.
The medicines that your rheumatologist prescribes will depend on your particular symptoms and how much pain and inflammation you have.
Your medicines may also change over time. Your rheumatologist might try different medicines to find out which will work best for you, or you may need an additional medicine if your condition or symptoms worsen.
Usually, you need to have tried a certain number of medicines before another is recommended for you. For example, bDMARDs are only prescribed if your RA is active and you haven’t had success with standard treatments.
You’ll need to see your doctor regularly for blood tests to see if the medicines are working for you and to monitor for side effects.
Exercise
This is one of the most important things you can do to manage your RA. Exercise can improve symptoms, including stiffness, pain, and fatigue, and reduce inflammation. It helps increase your flexibility and range of movement, so it’s easier to do many everyday activities.
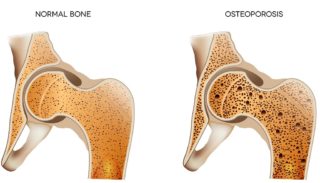
Being active is also essential for your overall health and wellbeing. It helps keep your muscles, bones and joints strong so that you can keep moving. It reduces your risk of developing other conditions such as heart disease, osteoporosis, and diabetes. It boosts your mood, benefits your mental health, helps with weight control and improves sleep.
Low-impact aerobic activities like exercising in warm water, cycling and walking can be a good place to start. Activities like strength training and tai chi are also beneficial. A physiotherapist or an exercise physiologist can give you information and support if you need help starting. They’ll also ensure you exercise safely to avoid injuring or straining your joints.
Self-care
There are other things you can do to manage your RA.
Learn about your condition. Understanding RA allows you to make informed decisions about your healthcare and actively manage it.
Manage your weight. Being overweight or obese increases inflammation throughout your body. This inflammation affects not only your joints but also your blood vessels and insulin levels. This can increase your risk of other chronic health conditions, including heart disease and diabetes. People with RA already have a higher risk of developing these conditions, so losing weight is an important thing you can do to reduce this risk. Being overweight or obese also limits the effectiveness of some medicines used to treat RA. Losing weight can be challenging, especially when pain impacts your ability to participate in physical activity. But it may help you to know that even a small amount of weight loss can help to improve your symptoms.
Learn ways to manage your pain. Pain is the most common symptom of RA, so it’s crucial to learn ways to manage it effectively. Read our A-Z guide for managing pain for more information.
Work closely with your healthcare team. The best way to live well with RA is by working closely with the people in your healthcare team (e.g. GP, rheumatologist, physio). Keep them informed about how you’re doing and if you’ve experienced any changes in your symptoms or tried new medicines, complementary therapies, supplements or other treatments.
Use aids and equipment. Supports such as long-handled shoehorns, reachers and canes can reduce joint strain and make life easier, especially if your condition has reduced your flexibility and mobility. An occupational therapist can advise you on aids, equipment and home modifications. You can also check out our range of aids in our online shop.
Protect your joints. Splints, orthotics and other supports may help reduce pain and prevent joint damage or inflammation. A physiotherapist or podiatrist can advise you on whether these strategies could be helpful for you.
Talk to an OT. An occupational therapist can advise on pacing yourself and managing fatigue, and how to modify your daily activities at home and work to reduce strain and pain on affected joints.
Sleep well. Not getting enough quality sleep can worsen your symptoms; however, getting a good night’s sleep when you have RA and chronic pain can be difficult. If you’re having problems sleeping, talk with your doctor about ways to deal with this. There are many options available to help you sleep better.
Manage stress. Stress can also aggravate your symptoms, so learning to deal with stress is extremely helpful. Things you can do to manage stress include planning your day and setting priorities, using relaxation techniques such as going for a walk, getting a massage or listening to music, and, where possible, avoiding people and situations that cause you stress.
Practise mindfulness. Regularly practising mindfulness meditation can improve your mood, relieve stress, improve sleep, improve mental health and reduce pain.
Eat a healthy, balanced diet. While there’s no specific diet for RA, it’s important to have a healthy, balanced diet to maintain general health and prevent weight gain and other health problems, such as diabetes and heart disease.
Quit smoking. Smoking cigarettes harms your general health, negatively affects your bone health, and increases inflammation. Smokers also have a greater risk of developing more severe RA, may be less likely to have remissions, and are more likely to have RA-associated lung disease. Smoking can make it more difficult to manage your pain. It causes fatigue and slower healing, which can make your pain worse. And it can make some of your RA medicines less effective. If you’re a smoker, you may be less likely to be as active, and less physical activity can increase your pain too.
What about surgery?
Surgery may be needed in some cases. Your doctor may suggest surgery as an option to:
- improve your joint movement
- improve your mobility and independence
- correct the position of joints that have become misaligned
- relieve pain that’s no longer controlled with treatments such as medicines, heat and cold, massage or exercise
- improve health and wellbeing if joint pain affects your sleep, mental health, and ability to work or participate in other important activities or events.
If your doctor thinks surgery might be a good option, they’ll refer you to an orthopaedic surgeon. Together, you can discuss the benefits and risks of surgery, alternatives and what will happen if you do nothing. You can then decide if it’s right for you. For more information, read Choosing Wisely Australia’s 5 questions to ask your doctor or other healthcare provider before you get any test, treatment, or procedure.
Contact our free national Help Line
Call our nurses if you have questions about managing your pain, musculoskeletal condition, treatment options, mental health issues, telehealth, or accessing services. They’re available weekdays between 9am-5pm on 1800 263 265; email (helpline@msk.org.au) or via Messenger.
More to explore