Rheumatoid arthritis (RA), osteoarthritis (OA) and osteoporosis (OP) have some similarities in their names, but is that where it ends?
This article will explore the similarities and differences of these common musculoskeletal conditions.
First – let’s look at those names
Rheumatoid arthritis – OK, this is a little convoluted, so hold onto your hat 😉. For those that don’t want the history lesson in ancient Greek, essentially it means inflammation of the joints. But for those who do read on…
Rheumatoid comes from rheumatism, which comes from the Greek word rheuma, which describes something that flows. Hippocrates (460-370BC), considered the father of modern medicine, ‘attributed many illnesses, especially those causing muscle achiness to the abnormal flow of body rheums or humors’.(1)
Arthritis – comes from the Greek word arthron for joint and itis, which means inflammation. Put together – inflammation of the joints.
Osteoarthritis – this is much more straightforward. Osteo – means bone and arthritis (inflammation of the joints).
Osteoporosis – another straightforward one 😉. Osteo (bone) and porosis means porous. So we have porous bones.
OK, we’ve had a trip through history and etymology, but what does this mean? I’ll admit rheumatoid had me scratching my head trying to work it all out. It seems to me that the rheuma part isn’t as helpful in the 21st century as it may have been for the ancient Greeks! But the arthritis part obviously is much closer to the mark. And you’ll see that the rest of the names pretty well match up with what’s going on with these conditions.
Rheumatoid arthritis (RA) vs osteoarthritis (OA) – what are the similarities and differences?
We know they’re both a type of arthritis. That’s the easy part. People who have these conditions will have some common symptoms – inflammation, joint pain and stiffness.
That’s about where the similarities end.
Rheumatoid arthritis is an ongoing health condition that causes pain, stiffness and swelling in your joints.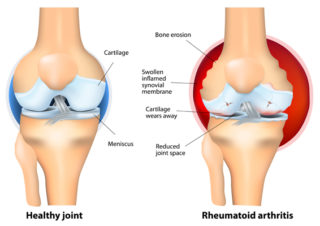
It’s the result of your immune system working in a faulty way. This is an autoimmune condition.
Your immune system is designed to look out for and attack foreign bodies – like bacteria and viruses – that can make you sick. For reasons that we don’t fully understand, when you have RA, your immune system gets confused. It targets your joints and healthy tissues as if they were foreign bodies.
This causes ongoing inflammation and pain.
Symptoms:
- swelling, pain and heat in the joints, usually the smaller joints of the hands or feet
- stiffness in the joints, especially in the morning
- persistent mental and physical tiredness (fatigue)
- same joints on both sides of the body are usually affected (symmetrical).
Less often, RA may also affect other systems in your body, like your eyes and lungs.
RA can affect people of any age but most often appears between 30 and 60. It affects women more often than men. However, when women reach menopause, the incidence of RA becomes the same for men and women.
How RA develops and how severe it is will be different for each person. Symptoms can develop gradually or can start with a sudden, severe attack. Your symptoms can change from day to day, and at times they can become much worse (called a flare). At other times, your symptoms may go away (called a remission).
The good news is that modern treatments for RA are extremely effective at controlling the disease and reducing its impact on people’s lives.
Osteoarthritis is the most common form of arthritis and affects the cartilage covering your bones’ ends.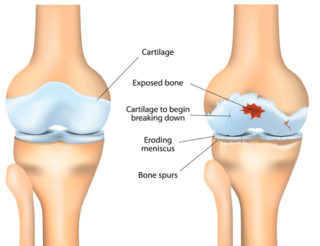
Healthy cartilage acts like a slippery cushion absorbing shock and helping your joints move smoothly. With OA, the cartilage becomes brittle and breaks down. Some pieces of cartilage may even break away and float around inside the joint. Because the cartilage no longer has a smooth, even surface, the joint becomes stiff and painful to move. Eventually, the cartilage can break down so much that it no longer cushions the two bones. Your body tries to repair this damage by creating extra bone. These are bone spurs. Bone spurs don’t always cause symptoms, but they can sometimes cause pain and restrict joint movement.
OA is most likely to develop in people over 45, but it can also occur in younger people.
Symptoms:
- joint stiffness
- joint swelling (inflammation)
- grinding, rubbing or crunching sensation (crepitus)
- joint pain
- muscle weakness.
It was once thought to be an inevitable part of ageing, a result of a lifetime of ‘wear and tear’ on joints. However, it’s now understood that OA is a complex condition and may occur due to many factors. The good news is that many of these factors can be prevented.
Treating RA and OA
Both rheumatoid arthritis and osteoarthritis can be managed effectively. Things you can do – whether you have RA or OA – include exercising regularly, maintaining a healthy weight (or losing weight if required), and taking any medicines as prescribed.
Treatment for rheumatoid arthritis will also focus on controlling your overactive immune system and preventing joint damage.
- Find out more about OA and the ways it’s treated.
- Find out more about RA and the ways it’s treated.
What about osteoporosis (OP)?
Osteoporosis doesn’t affect the joints as OA and RA do. It affects the bone itself. 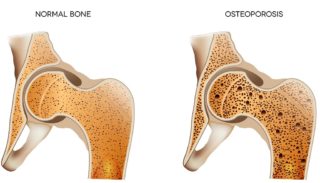
Bones are living tissue that’s constantly growing, rebuilding, replacing and repairing. From birth to about 25 years of age, you build more bone than you lose. Your bones are not only getting bigger as you grow during this time, but they’re developing their density. This determines how strong they are.
From about 25 to 50 years of age, your bones break down and rebuild at about the same rate. They’re in a state of balance. This is when you’ve achieved your ‘peak bone mass’. Your bones are at their strongest.
After about 50 years of age, you start to break down more bone than you rebuild. While this means that we’ll all experience some bone loss, it doesn’t mean that everyone will develop osteoporosis.
Women commonly experience a period of rapid bone loss after the onset of menopause. After this time, there’s a steady but less rapid loss of bone.
When a person develops osteoporosis, their bones become more porous, lose strength and become fragile. Osteoporotic bones break (or fracture) more easily than normal bones. Even a minor bump or fall can cause a serious fracture.
Many people with osteoporosis don’t know they have it. It doesn’t have any obvious signs or cause pain unless a bone has broken.
Common risk factors for osteoporosis include a family history of OP, having conditions such as RA, coeliac disease or diabetes, smoking, and not getting enough calcium or vitamin D. You can check if you’re at risk of OP by using the Know Your Bones online tool.
Treating osteoporosis
OP can also be effectively managed and involves regular weight-bearing exercise and a healthy diet incorporating calcium-rich foods. Depending your age, general health and fracture risk, your doctor may prescribe medicines to help slow down bone loss or increase the amount of bone that’s made. Find out more about OP and the ways it’s treated.
More to explore
- How are rheumatoid arthritis and osteoarthritis different?
healthline - Patient education: Osteoarthritis symptoms and diagnosis (Beyond the Basics)
UpToDate - Patient education: Osteoarthritis treatment (Beyond the Basics)
UpToDate - Patient education: Osteoporosis prevention and treatment (Beyond the Basics)
UpToDate - Patient education: Rheumatoid arthritis symptoms and diagnosis (Beyond the Basics)
UpToDate - Patient education: Rheumatoid arthritis treatment (Beyond the Basics)
UpToDate - Risk factors
Healthy Bones Australia - What’s the difference between rheumatoid arthritis and osteoarthritis?
Medical News Today
Reference
(1) How rheumatism got its name
The Rheumatologist




















